Globally, stunting is a common malnutrition health problem among children. In 2019, the prevalence of stunting was around 21.3% (UNICEF, 2020). Commonly found in Low-Middle-Income-Countries (LMICs), the highest prevalence of stunting occurs in Madagascar (49.8%), Guatemala (47%), Niger (47.5%), Burundi (54%), Madagascar (49.8%), Timor-Leste (49.8%), and Yemen (45.4%) (Kinyoki et al., 2020). The prevalence of stunting among children in Indonesia has been fluctuating. Recently, the prevalence of stunting was reduced from 37.2% (2013) to 30.8% (2018) (Indonesian Ministry of Health, 2018). Indonesia is still ranked second in South East Asia after Cambodia, which is based on the World Health Organization (WHO) ’s indicators, where the countries with a prevalence of more than 20% indicate the chronic stunting condition.
Stunting has a long-term effect on growth and development. Previous studies found that the most impact of stunting involved lower cognitive development, school achievement, and economic productivity during adult and maternal reproduction health (Woldehanna et al., 2017; Alam et al., 2020). In addition, stunted children under two years old are more susceptible to suffer infection and diseases.
Review studies found some factors that contributed to the stunting of Indonesian children. These included male, premature birth, short birth length, maternal height, low maternal education, low household economic status, untreated drinking water, poor access to health care, living in a rural area, number of the household member under 5-year-old, weight at birth, and number of antenatal care (ANC) visits (Beal et al., 2018; Nshimyiryo et al., 2019; Titaley et al., 2019).
Recent research found that the most important factor affecting stunting was the maternal education level. Mothers with a lack of formal education were more likely to have stunted children (Berhe et al., 2019). In collaboration with The United Nations International Children’s Emergency Fund (UNICEF), the WHO developed the Care for Child Development (CCD) program. This program aims to improve the mother’s (caregivers’) capability to be more sensitive and responsive to promote psychosocial development in young children (Chung et al., 2017). The CCD intervention has been piloted in 19 countries. However, only three countries implemented it as a national health policy that integrated the CCD with the health sector (Lucas et al., 2018). For example, in Pakistan, CCD interventions that involved Lady Health Workers (LHW) have enhanced the nutritional status among children under four years (Yousafzai et al., 2016).
In Indonesia, the large geographic diversity leads to inequality in many aspects of health care services, including access and coverage (Al-Ashwal et al., 2020). In 2018, the ratio of nurses for 1,000 population in Indonesia was 2.41 (The World Bank, 2021), which is less than what is recommended by the Organization for Economic Co-operation and Development (OECD) (OECD, 2019). In addition, most nurses are working in the hospital setting, and only a limited number of nurses are working in the community. Nurses working in Public Health Centers (Puskesmas) are responsible for monitoring children’s health, growth, and development. Due to the limited number of nurses, they often involve cadres (LHW). Usually, the cadres in every village can routinely monitor children’s nutritional and developmental status through community programs such as Balita, which are focused on children <5 years old (Solikhah et al., 2018). Nurses from the local Puskesmas are responsible for providing training and supervising the volunteer cadres. The CCD program is essential to improve the Knowledge, Attitude, and Efficacy (KAE) of cadres. It will increase cadres’ capability to fulfill their role as health educators and health facilitators in the community. However, the CCD intervention needs modification according to cadres’ culture and local wisdom or mothers/parents in the community. The local wisdom approach will help cadres adapt their strategy and reach the goals of CCD training (Yousafzai et al., 2016). Recent research has shown that cultural involvement in training improved cadre’s knowledge, attitude, and skills in the community (Subandi et al., 2019). In this study, the CCD intervention was modified by adding traditional games, Javanese music, and local forms of advice-giving. This study aimed to assess the effect of the CCD training on cadre’s knowledge, attitude, and efficacy about stunting, in Yogyakarta, Indonesia.
Methods
Study Design
We conducted a community-based study with a quasi-experimental research design using a comparison group from March 2018 to February 2019.
Study Setting and Participants
The study was conducted in Yogyakarta Special Province, Indonesia. Yogyakarta Special Province consists of five districts: Kulon Progo, Sleman, Gunung Kidul, Bantul, and Yogyakarta City District. In 2019, the Kulon Progo District had the second highest ranked prevalence of stunted children (Health District Yogyakarta Province, 2019). From 12 sub-districts, Samigaluh and Kalibawang sub-district had the highest prevalence of stunting in their population. Both sub-districts are rural and remote areas.
Puskesmas serves as the first gate to access health care services in Indonesia. In Kulon Progo District, there are 21 Puskesmas, and each has a responsibility to cover a minimum of 30,000 population. Based on the current data from the Health District Yogyakarta Province, the highest number of stunted children were found in the areas covered by Puskesmas Kalibawang, Puskesmas Samigaluh I, and Puskesmas Samigaluh II. For sustainability, the community health nurses should regularly collaborate with cadres to improve the nutrition status of the children in their area. Therefore, we recruited cadres who are working under the supervision of nurses from those three Puskesmas. The cadres are healthcare volunteers who have a responsibility to support health programs in the community. Most of them are women who live in their village, and they do not receive a salary.
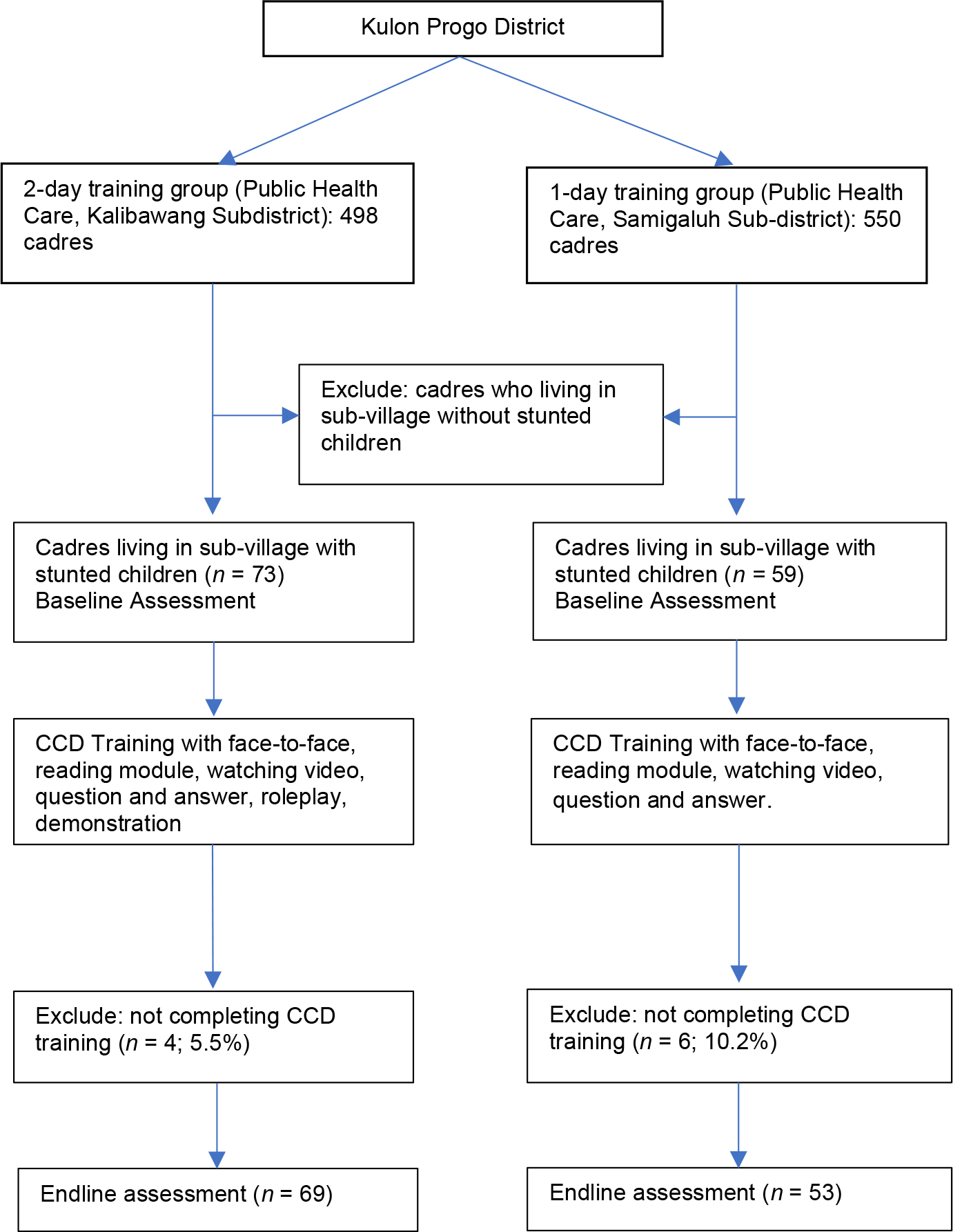
Cadres living in Kalibawang were assigned as the two-day training group, and cadres living in Samigaluh were selected as the one-day training group. The convenience sampling method was used with the following inclusion criteria: registered cadres in the Puskesmas, minimal education background of Junior high school, living in sub-village with stunted children < 2 years old, and agreed to participate in the program. The details of the participant selection are shown in Figure 1.
Instruments
We collected data concerning the basic characteristics of participants, including age, educational background, duration as cadres, and quantity of training. The knowledge data described the knowledge of cadres related to children’s development, how to give children stimulation, and how to educate mothers about how to do mother-children interaction according to their development stage. The knowledge of cadres was evaluated by the Caregiver Knowledge of Child Development Inventory (CKCDI), consisting of 20 questions (Ertem et al., 2007). The Indonesian version of the CKDI has been culturally and linguistically validated (translated and back-translated). The Cronbach alpha of the knowledge instrument was 0.820. The range score is 0 ~ 40, with the higher score indicating more knowledge (Shrestha et al., 2019).
Attitude mainly describes how the cadres respond appropriately, including how to provide support or not through children development counseling. We developed a questionnaire to assess the cadres’ attitude, modified from the WHO’s CCD guideline (WHO, 2012). It consists of 19 items with a Cronbach alpha of 0.831. The range score of 4~ 76. A higher score indicates a higher attitude.
The cadres’ efficacy was a measure of the cadres’ confidence to educate primary caregivers regarding the stimulation of children’s development. We used the validated Indonesian version of the General Self-Efficacy Scale (GSES) to evaluate the efficacy of cadres. GSES was developed by Schwarzer and Jerusalem in 1995 (Schwarzer & Jerusalem, 1995). The Indonesian language version is available on the following website: http://userpage.fu-berlin.de/%7Ehealth/indonese.htm. It uses a Likert scale, and the result of the internal validity test was 0.725. The range of total score 10 ~ 40. A higher score indicates a higher efficacy.
Data Collection
The study process is described below:
1. Pre-intervention phase
In this phase, the researchers identified people involved in this study, such as instructors, facilitators, and enumerators. Instructors have a task to deliver the training material to cadres. Instructors were nurses from the School of Nursing Universitas Gadjah Mada, Yogyakarta, with master’s or doctoral education backgrounds. Facilitators were selected from community health nurses from the three Puskesmas. Facilitators had the tasks to support the demonstrations during the training process, while enumerators had to collect the data before and after the intervention. All instructors, facilitators, and enumerators were trained before the implementation of the study.
The research team developed a training module based on the WHO CCD guideline. We modified it to the culture and local wisdom of cadres or mothers/parents in the community. The module was complemented with video, PowerPoint (PPT) presentation, and local toys. All of the local toys were adopted from Javanese culture. The module consists of a pocketbook and counseling card. The topics covered in the module included: who has the responsibility to care for the children; child development care; how to use counseling cards; recommendation for child development care; advice to improve communication and play, and how to create toys for playing. Additional topics included: family counseling how to child development care; how to observe, listen, and ask questions to make accurate child development care identification; how to give feedback, advice, and reinforcement to mother (caregivers); how to create a follow-up for child development care problems; and how to deliver counseling and help solve any issues. The module was piloted before the study implementation.
2. Intervention phase
The CCD training for the intervention group lasted two days. On the first day, the training methods in this group were reading the module, watching a video, demonstrating, and role-playing. On the second day, all cadres showed the counseling practice to a mother under the supervision of instructors. In this step, each cadre provided counseling to five mothers. The cadres received the CCD introduction, then watched the educational video and engaged in small group discussion.
Before the training started, questionnaires for the pre-test were distributed to participants, and questionnaires for the post-test were distributed three weeks after the training program. The CCD training was conducted in each village office. The training activities are described in Table 1.
| Intervention / Two-day training group | Comparison/One-day training group | |
|---|---|---|
| Training media | CCD module | CCD module |
| Pocketbook | - | |
| PowerPoint | PowerPoint | |
| Video | Video | |
| Checklist sheet | Checklist sheet | |
| Sticky sheet | Sticky sheet | |
| Stimulation kit | - | |
| Instructure | 5 Nurses | 5 Nurses |
| Facilitator | 7 Nurses | 7 Nurses |
| Delivery method | Face-to-face training | Face-to-face training |
| Reading module | Reading module | |
| Watching video | Watching video | |
| Question and answer | Question and answer | |
| Role-play | ||
| Demonstration | ||
| Duration | 10 hours | 5 hours |
| Evaluation method | Direct feedback | Direct feedback |
| Questionnaires | Questionnaires | |
| Redemonstration |
Data Analysis
Descriptive statistics were used to describe the distribution, frequency, and percentage of variables with means and standard deviation (SD). The comparisons of participants’ levels of knowledge, attitude, and efficacy between pre-and post-intervention in each group were assessed using nonparametric Mann-Whitney U tests. For comparison analysis of pre-and post-intervention results between the two groups, we used Wilcoxon Sign tests. P-value less than 0.05 indicated statistical significance. All analyses were performed using SPSS for Windows version 19 (SPSS, Chicago, IL, USA).
Ethical Consideration
This study was approved by the Medical and Health Research Ethics Committee (MHREC) Faculty of Medicine Gadjah Mada University-Dr. Sardjito General Hospital with number: KE/FK/0145/EC/2018. Informed consent was obtained from all participants. Firstly, we explained the purpose, the process of the study, and the benefits for the participants. Secondly, we provided time for the participants to clarify or ask questions related to the study. Finally, written informed consent was obtained from all participants before the study was conducted.
Results
Table 2 shows the basic characteristics of participants. The mean age, duration experiences as cadres, and training frequencies were closely similar in both groups. However, the educational background was significantly lower in the two-day training group than in the one-day group.
| Intervention group (n = 69) | Comparison group (n = 53) | p-value | |
|---|---|---|---|
| Mean ± SD (%) | Mean ± SD (%) | ||
| Age (year) | 42.09 ± 8.37 | 41.26 ± 7.88 | 0.818a |
| Educational background | |||
| Junior high school | 50 (72.5%) | 22 (41.5%) | 0.001*b |
| Senior high school and above | 19 (27.5%) | 31 (58.5%) | |
| Experience as cadres (year) | 9.93 ± 8.08 | 11.93 ± 8.10 | 0.157a |
| Quantity of training | 3.65 ± 1.62 | 3.64 ± 1.62 | 1.000a |
Table 3 shows the comparison of the participants’ levels of knowledge, attitude, and efficacy in intervention and comparison groups at the baseline and the end of the training period. At the baseline, the knowledge of both groups was significantly different. The mean of knowledge in the intervention group was slightly higher than the comparison group. After the intervention, the knowledge of both groups was still significantly different. However, the level of efficacy was only significantly different between the intervention group and the comparison group in the post-intervention scores.
| Intervention group (n = 69) | Comparison group (n = 53) | p-value | |
|---|---|---|---|
| Median (min-max) | Median (min-max) | ||
| Pre-Intervention | |||
| Knowledge | 11 (7~16) | 10 (7~14) | 0.027* |
| Attitude | 55 (36~75) | 57 (47~69) | 0.159 |
| Efficacy | 28 (10~37) | 27 (19~34) | 0.120 |
| Post-Intervention | |||
| Knowledge | 14 (9~16) | 12 (4~18) | 0.001*** |
| Attitude | 58 (50~74) | 57 (49~70) | 0.16 |
| Efficacy | 30 (23~39) | 29 (21~40) | 0.017* |
Table 4 shows the comparison of pre-test and post-test scores in both groups. The mean scores before and after CCD training in the intervention group were significantly increased for all outcomes: knowledge, attitude, and efficacy (p <0.001). However, the scores of the comparison group increased only for knowledge and efficacy (p <0.001). Table 5 shows the comparison effect of CCD intervention on knowledge, attitude, and efficacy between the intervention and the comparison group groups. The score change or delta before and after CCD training for attitude in the intervention group was significantly higher than the comparison group (3.78 vs. 0.72; p = 0.05).
| Variables | Pre-test | Post-test | p-value |
|---|---|---|---|
| Median (min-max) | Median (min-max) | ||
| Intervention Group | |||
| Knowledge | 11 (7~16) | 14 (9~16) | 0.001*** |
| Attitude | 55 (36~75) | 58 (50~74) | 0.001*** |
| Efficacy | 28 (10~37) | 30 (23~39) | 0.001*** |
| Comparison Group | |||
| Knowledge | 10 (7~14) | 12 (4~18) | 0.001*** |
| Attitude | 57 (47~69) | 57 (49~70) | 0.255 |
| Efficacy | 27 (19~34) | 29 (21~40) | 0.001*** |
Note: * p <0.05; ** p <0.01;
Discussion
This study aimed to identify the effect of culturally adapted CCD training on cadres’ knowledge, attitude, and efficacy. Results indicated that CCD training significantly increased cadres’ knowledge, attitude, and efficacy in the two-day training group. In the comparison group, the CCD training significantly improved cadres’ knowledge and efficacy but not their attitude. The final results show that the delta score before and after CCD training for cadres’ attitude in the intervention group was significantly higher than that of the comparison group.
For cadres’ knowledge, the mean difference was slightly higher for the two-day training group than that of the comparison group because the education background of cadres in the one-day training group was higher, and their experience was longer than that of the intervention group. This is the possible reason why the knowledge of both groups differed slightly. The previous study found that the higher education background in health volunteers will help them better understand new information. Therefore, they will easily improve their performance as health volunteers (Chung et al., 2017). The differences between learning methods for both groups also contributed to the different knowledge scores for both groups. However, in the final result, this was not significantly different. So, we assume that all participants had enough resources, appropriate learning methods, and had enough time to practice the material by themselves. Therefore, the learning methods of CCD training in this study for the two groups can be implemented for cadres in the community. One previous study stated that the role-play method was more effective in increasing knowledge (Vizeshfar et al., 2019). Considering the duration of intervention, another study found that it was significant in increasing the participants’ knowledge between intervention and control groups. The knowledge score was higher in the group that received a more extended training duration (Tambi et al., 2019).
However, in this study, the two-day and one-day interventions have similar increases in the knowledge of cadres. Another possible reason for this result is the CCD training had already been adapted into the participants’ culture and local wisdom. The culture approach reduced the barriers of interaction between instructors and cadres during the intervention. Cultural awareness is considered an important factor when the researcher adapts some health guidelines into a community (Shepherd et al., 2019). The CCD training in this study was only adapted for the Javanese culture. These results also serve as a reminder for the health workers or leaders in the community that they should be sensitive to various Indonesian cultures. Overall, the increasing knowledge in the CCD training is vital to increase awareness of cadres about the stunting children in their community (WHO, 2012).
We found the cadres’ attitude was significantly higher in the intervention group than that for the comparison group. This result may occur due to the different learning methods. One study found that a better mood increased the motivation of the students to study and improve their cognitive capacity (Forbes & Schmader, 2010). The increasing of knowledge in this result had the primary goal to increase the attitude of cadres. It was consistent with the previous study that found the levels of knowledge and attitude were strongly linear (Muleme et al., 2017). For the delivery of health education in the community, the attitude of cadres becomes a motivation to deliver health education to mothers in the community. In the CCD intervention, their willingness develops into good behavior during the interaction between cadres and mothers or parents in the counseling section.
Besides that, the methods of CCD training in this study also used role-play and demonstration. Using role-play is known to increase participants’ attitudes and knowledge compared to the lecturer method (Wang et al., 2015). The benefits of role-playing and demonstrations were to reduce the boredom of the audience and increase the enthusiasm in their attitude. Notably, these methods use more sense of body language and going through the motions to receive the new information. However, the use of role-playing and redemonstration was time-consuming (Vizeshfar et al., 2019).
The increase of the cadres’ efficacy is part of the main goal of the study. The efficacy score of CCD training increased before and after intervention for both groups. However, the efficacy of volunteer health workers is influenced by their knowledge and attitude (Zamani-Alavijeh et al., 2019). The people who have good efficacy will generally be confident and successful in communicating with other people. They will efficiently deliver the information to other health volunteers (Alber et al., 2016). Therefore, efficacy is an essential factor to consider in performing as a health educator.
An important aspect of the efficacy’s concept is vicarious experience when they get new information from observation activity. This concept was successfully implemented in the CCD training. Demonstrations and role-plays are appropriate delivery methods in the intervention. It allows participants to increase their efficacy. During the intervention, participants can observe responses from the trainer, mother or parent, and children. In general, good efficacy contributes to the cadres’ performance. However, some additional factors influence the efficacy. A previous study stated that some influencing factors were the quantity and quality of the training (Zamani-Alavijeh et al., 2019). Related to the characteristics of the participants in this study, the results showed that they had a similar quantity of training, although the duration of experience as cadres was slightly different. For quality, this study tried to combine face-to-face, demonstration, and role-play for learning methods. Results showed a slightly higher change of efficacy in the intervention group compared to the control group. Several factors, such as encountering unexpected events, can cause self-efficacy reduction. Typically, vicarious experiences, self-concept, and self-efficacy act as reciprocally interacting influences on a person’s perception of trust, while professional knowledge and skills also are known to increase efficacy.
Our results show that the CCD training can be implemented for cadres in Indonesia. The increasing number of cadres with CCD training experience is expected to create better health educators for mothers or parents with stunted children in the community. This study’s implications support how cadres’ role can increase nutrition status among children in the community with supervision by community health nurses from Puskesmas. This improvement in nutrition is an essential part of the role of the nurses especially related to community health empowerment activities. Therefore, the Indonesian Government should support and facilitate the current and continuous training for cadres in the community.
Strengths and limitations
As far as our knowledge, this was the first study to examine the effect of culturally modified CCD intervention training among cadres in rural areas, especially on knowledge, attitude, and efficacy. Nevertheless, this study has some limitations. First, the study was not a true experimental design. The selection bias of participants was possible in this study. Further study with a randomized control trial is needed. Second, we only assessed the knowledge, attitude, and self-efficacy only one time after the intervention. Finally, the material of CCD intervention was adapted for Javanese culture. Accordingly, when other researchers want to adapt the material, they should be sensitive to the culture of the cadres’ life.
Conclusion
A culturally modified CCD training significantly improved cadres’ knowledge, attitude, and efficacy in the intervention and control groups. In addition, the learning delivery method with demonstrations and role-plays significantly improves cadres’ attitudes as health educators for stunted mothers or parents in the community. For sustainability, the community health nurses should regularly meet with cadres to maintain their current knowledge, attitude, and efficacy.