Over the past three decades, evidence-based application of nursing practice has come into sight as a significant matter to clinical nursing practice and the health care system (Alqahtani et al., 2020; Pierce, 2020). Evidence-based nursing practice has been defined as an ideal problem-solving approach and practice of the best evidence derived from well-designed research projects concerning nursing inquires of the patients, their preferences, and values (Jolley, 2020). The importance and cost-effectiveness of evidence-based practice have been extensively discussed in the nursing literature since it has an immediate impact on patients, nurses, and the health care system (Squires et al., 2011; Williams et al., 2015; Cheng, Feng, et al., 2017). Evidence-based practice is necessary because it can reduce cost, save time and result in better patient outcomes (Cheng, Feng, et al., 2017; Jolley, 2020).
In today’s healthcare environment, the urgent call to provide high-quality nursing care has been growing worldwide. The profession of nursing is one of the major health professions that could significantly impact healthcare quality (Pierce, 2020). Therefore, governmental and private agencies in the Kingdom of Saudi Arabia (KSA) recommend improving evidence-based competencies for nurses to guarantee superior nursing care (Hasheesh & AbuRuz, 2017). Evidence-based nursing competencies have been praised and mandated as the heart of evidence-based nursing (EBNP) (Pierce, 2020). The recent emphasis in the KSA is for a health care system that is up to date, trustworthy, and offers quality-guaranteed services (Hasheesh & AbuRuz, 2017). The dynamics for high-quality nursing care have begun to be increasingly substantial in the Saudi Health Care System (SHCS) (Hasheesh & AbuRuz, 2017; Mohammed Hamdan et al., 2020). Considering nursing paradigms shift to evidence-based care, Saudi nursing professionals have launched significant efforts to establish their own existence in the evidence-based world (Hasheesh & AbuRuz, 2017).
However, despite widespread demands to incorporate evidence-based principles in clinical practice, evidence-based implementation has been slow and inconsistent (Cheng, Feng, et al., 2017; Ellis, 2019; Alqahtani et al., 2020). Worldwide, several studies conducted in a variety of countries showed that the application of the evidence-based approach is a complex activity (Al-Momani et al., 2016; Ellis, 2019; Abuejheisheh et al., 2020; Alqahtani et al., 2020). Therefore, to understand the multifaceted evidence-based practice implementation process, it is necessary to investigate factors that enable successful evidence-based implementation (Ellis, 2019).
Previous studies have tackled the multitude of influencing personal and organizational factors on evidence-based practice implementation (Leung et al., 2016; Cheng, Broome, et al., 2017). Cheng, Broome, et al. (2017) and Leung et al. (2016) found that lack evidence-based knowledge and skills, such as the skills of clinical question identification and formulation, relevant evidence searching, critical literature appraisal, and evidence integration and implementation. However, other researchers found that knowledge and skills are not necessarily enough to engage nurses in the process of evidence-based nursing application (Hasheesh & AbuRuz, 2017; Alqahtani et al., 2020). Pierce (2020) highlighted the importance of attitudes in changing nursing practice.
Building on the work of previous researchers, there have been numerous studies conducted to examine the impact of personal factors such as evidence-based competencies, attitudes, and beliefs related to the evidence-based application (Farokhzadian et al., 2015; Leung et al., 2016; Cheng, Broome, et al., 2017).
Recently, literature has gradually shifted from personal factors to organizational factors (Williams et al., 2015; Ellis, 2019; Lizarondo et al., 2019; Boltz et al., 2020). The literature identified potential organizational barriers that impact nurses’ ability to promote and maintain evidence-based approach, that is, (a) lack of time, (b) lack of staff/administrative support, (c) resources deficiency, (d) absence of autonomy and power to change practice and (e) resistance to change (Williams et al., 2015; Al-Momani et al., 2016; Johnston et al., 2016; Cheng, Broome, et al., 2017).
On the other hand, Duncombe (2018) identified potential organizational facilitators that enhance nurses’ ability to promote and maintain evidence-based approach, that is, (a) managerial support, (b) accessibility to articles, (c) comprehension of scientific research, (d) availability of time to read and utilize research results, and (e) adequate authority over practice (Duncombe, 2018). Bearing in mind the sophisticated nature of the evidence-based nursing practice, manipulating only personal factors might not be adequate to promote the evidence-based application.
Hence, the assessment of personal and organizational factors on several levels simultaneously is essential to study their complex interactions (Cheng, Broome, et al., 2017). A large body of literature has discussed a wide range of factors that have a great influence on EBNP; these include as perceived by registered nurses : (a) evidence-based practice competencies (Connor et al., 2017; Hasheesh & AbuRuz, 2017), (b) evidence-based practice beliefs (Cruz et al., 2016; Laske & Kurz, 2019), and (c) evidence-based practice facilitators and barriers (Johnston et al., 2016; Spooner et al., 2018; Lizarondo et al., 2019). Although considerable literature examining factors influencing the implementation of EBNP in clinical practice is widely present internationally (Barako et al., 2012; Bostrom et al., 2013; Farokhzadian et al., 2015; Kim et al., 2015; Park et al., 2015; Cheng, Broome, et al., 2017; Connor et al., 2017), only a few studies had been conducted in Saudi Arabia to address those factors (Cruz et al., 2016; Hasheesh & AbuRuz, 2017; Alqahtani et al., 2020). In addition, the majority of these studies focused on either personal or organizational factors without considering their complex interaction (Cruz et al., 2016; Hasheesh & AbuRuz, 2017; Alqahtani et al., 2020).
Moreover, there is still a huge gap between nurses’ evidence-based knowledge and what is truly done in recent nursing practice (Cheng, Broome, et al., 2017). Therefore, it is essential to identify all potential factors that could interfere with evidence-based practice implementation (Johnston et al., 2016; Kang & Yang, 2016; Connor et al., 2017). To date, only one study has used a conceptual model to explain the predictive effect of a limited set of organizational and personal factors (De Pedro Gomez et al., 2012). Comprehensive assessment of these factors using a valid conceptual model can help develop appropriate interventions to promote evidence-based practice in clinical practice. To our best knowledge, a valid conceptual model that adequately explains a set of factors associated with the application of evidence-based practice has not been available. Therefore, the aims of the current study were to generate and validate a model of factors significant to and predictive of the application of evidence-based practice.
Conceptual Model Development
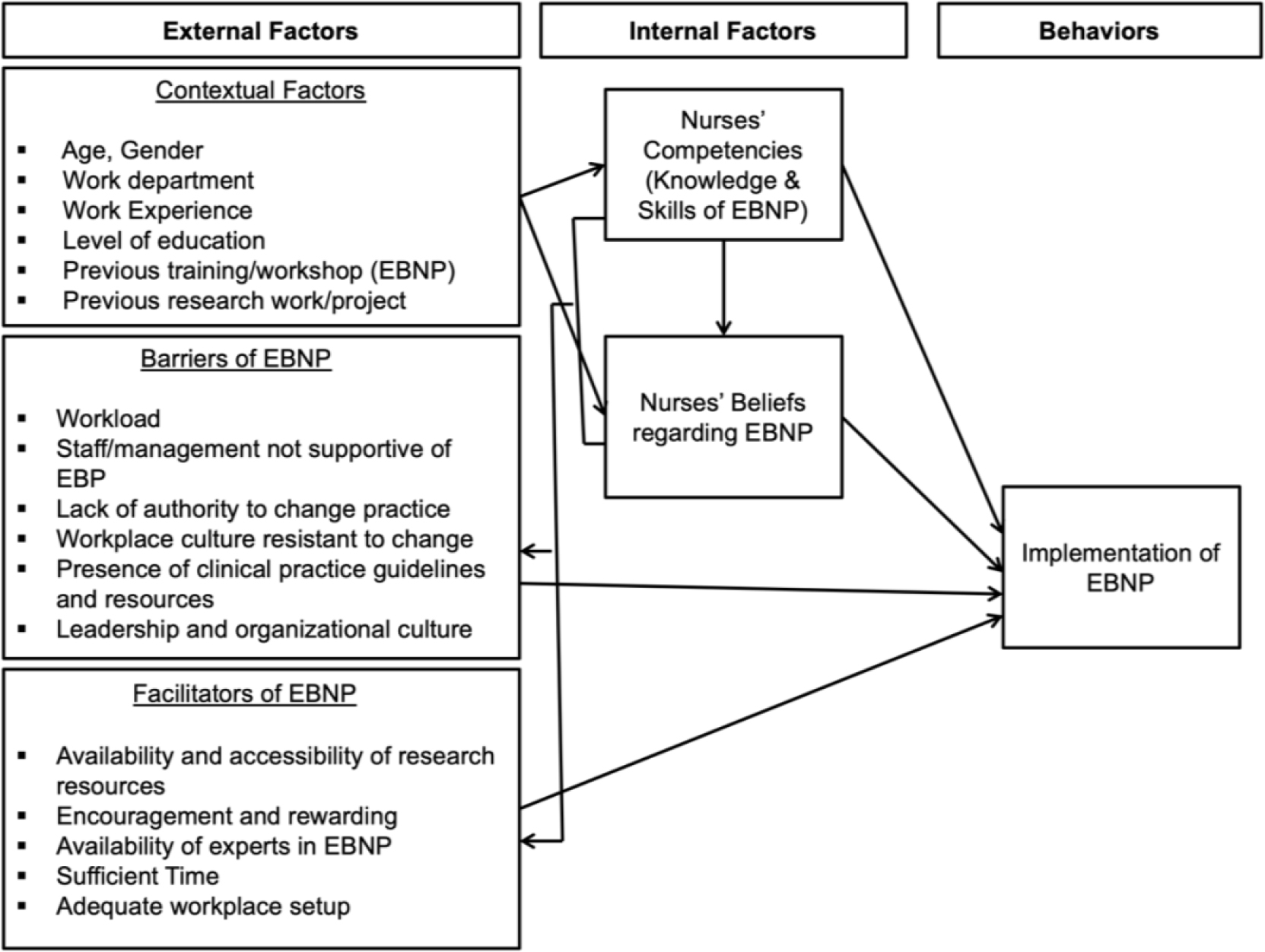
The current study used a hypothetical conceptual model that was derived from previous literature (Park et al., 2015; Al-Momani et al., 2016; Hellier & Cline, 2016; Cheng, Broome, et al., 2017) and a concept analysis study that investigated the hypothetical relationships between the antecedents, attributes, and the consequences of evidence-based practice implementation (Chiwaula et al., 2018).
According to the literature, five essential domains were recognized to influence the evidence-based implementation. The review identified nurses’ competencies, beliefs, facilitators, barriers, and contextual attributes as important domains. These five domains create the conceptual model structure. In the Oxford dictionary, competence is described as “the ability to do something well”; beliefs as “a strong feeling that something is true”; facilitator is defined as “person or (factor) who (which) helps somebody do something more easily by discussing problems, giving advice, etc. rather than telling them what to do”; barrier is described as “problem, rule or situation that prevents somebody from doing something, or that makes something impossible”; and implementation as “the process of putting a decision or plan into effect; execution” (Stevenson, 2010).
These definitions relate to the conceptual model as follows: competence reveals a nurse’s cognitive ability to perform a task, incorporating attributes of knowledge and skill related to EBNP (Leung et al., 2016); beliefs as to endorse the idea that EBNP improves patient outcomes and being confident in one’s knowledge or skills about EBNP (Laske & Kurz, 2019); barriers, as all elements that inhibit the nurses’ ability to use research evidence in their practice (Johnston et al., 2016); facilitators, as all elements that help the nurses’ ability to use research evidence in their practice (Johnston et al., 2016); and implementation, as the application of evidence-based process steps (Connor et al., 2017). These factors are related to each other and may work together to affect the application of evidence-based practice (Hellier & Cline, 2016). In addition, some factors contain several interrelated sub-factors (contextual factors) that must be considered (Chiwaula et al., 2018). The current study used a researcher-constructed structural model (See Figure 1).
This model is composed of five domains (evidence-based practice barriers, facilitators, competence, beliefs, and contextual variables) that might impact the application of evidence-based practice. Contextual factors are presented in seven variables (age, gender, department, experience, education, previous training/workshop, and previous research work).
Methods
Design
A descriptive (cross-sectional) design was used in the current study. Structural equation modeling (SEM) is used to estimate causality and relationships of multiple independent and dependent variables simultaneously. This method also aids in identifying direct, indirect, and total effects (Schermelleh-Engel et al., 2003).
Sample and Setting
Six hundred and twelve registered nurses were enrolled using a convenience sampling procedure from four hospitals. The author used an algorithm calculator invented by Westland (2010) to compute the required sample size; assuming (β= .80), (α=.05), medium effect size (f2 = .3), and five latent factors would require at least two hundred subjects to discover the effect (Westland, 2010). The study sample included registered nurses from the in-patient surgical, medical, and critical care units, having previous clinical experience of more than twelve months, and consenting to join. Contacting representatives with hospitals approached and screened the subjects for eligibility.
Instrument
A two-part self-report questionnaire was used to collect data. The first part of the questionnaire was used to gather information on contextual variables such as level of education, age, gender, experience, department, exposure to previous evidence-based practice training/workshop, and conducting or participating in any previous research project/activity.
Evidence-based competencies, beliefs, facilitators, barriers, and implementation were measured using Registered Nurses’ Competencies, Beliefs, Facilitators, Barriers, and Implementation of Evidence-based Practice Questionnaire (EBP-CBFRI Questionnaire) developed by Abuadas et al. (2021). The questionnaire is composed of 55-items distributed within five subscales; perceived competencies (14 items), beliefs (10 items), facilitators (9 items), barriers (10 items), and implementation (12 items). Each item was scored on a 5-point Likert-type format, ranging from 1 (strongly disagree) to 5 (strongly agree). The overall validity of the questionnaire was established based on the S-CVI score, which was .92. As well as, the I-CVI confirmed that all items were scored as acceptable (values ranged from .83-1.00). Cronbach’s alpha was .87 for the overall questionnaire and ranged between .92 and .95 for all five subscales. All the corrected item-total correlations were found to be >.30 and ranged from .66 to .78. The EBP-CBFRI questionnaire had good internal reliability and validity since it showed satisfactory evidence of content, construct, convergent, and discriminant validity when used with registered nurses in Saudi Arabia (Abuadas et al., 2021).
Data Collection
Permission was obtained from hospital administrators prior to data collection. Data were collected between November 2019 and January 2020 in the inpatient medical-surgical units and critical care units. After receiving permission, data collectors approached the nurses in their wards. Nurses approved to take part were given the questionnaires enclosed with the consent form. Finally, the data collectors gathered the completed questionnaires after allowing adequate time for subjects. On average, it took about 25 minutes to complete the whole questionnaire.
Data Analysis
Participants’ demographic characteristics frequencies, percentages, means, and standard deviations were described using descriptive statistics. Structural equation modeling was used to find the direct, indirect, and total effects of the contributing factors and build a preliminary hypothetical model of evidence-based practice implementation among the nurses. Relationships between the variables/factors were estimated using Pearson’s correlation coefficients. Maximum likelihood estimation was used to estimate parameters and test the path validity. The current study used the thresholds of fit recommendations for Schermelleh-Engel et al. (2003) to assess the model fit as follow: (i) a critical ratio (CR) >1.96 of factor loadings, (ii) relative Chi-Square (𝜒2/df) ≤5, (iii) the normed fit index (NFI) and the comparative fit index (CFI) ≥.85, (iv) adjusted goodness of fit index (AGFI) and the goodness of fit index (GFI) ≥.85, (v) the standardized root mean square residual (RMR) and root mean square error of approximation (RMSEA) ≤.08 (Schermelleh-Engel et al., 2003). Prior to the model development, the author checked for normality, independence, and homoscedasticity. Random missing data were replaced using the case mean imputation approach.
Ethical Considerations
Approval from the Institutional Review Board (IRB) was attained prior to data collection (the approval no. HA-06-B-001 ECM#2019-44). At the beginning of the survey, detailed written information was provided, and the participants were informed that the participation was voluntary and anonymity was maintained. The consent form was enclosed with each questionnaire.
Results
Characteristics of Participants
The current study showed a response rate of (77%); a total of 612 nurses returned completed questionnaires. The mean age was 31.86 years and a standard deviation of 6.79 years. The standard deviation ranged between 24 and 45 years. In addition, the participants consisted of females (57%) and 4males (43%). Nurses’ experience mean was 6.73 years with a standard deviation of 2.39 years. The bulk of the sample underwent undergraduate education (84.5%). Being engaged in previous evidence-based workshops or training was reported in more than half of the participants (69.8%). Regarding the engagement in medical or nursing research studies, only a few participants (25.3%) were involved in medical or nursing-related studies throughout the past years (See Table 1).
| Variables | N | % |
|---|---|---|
|
Gender Male Female |
263 349 |
43% 57% |
|
Level of education Bachelor level Master level |
517 95 |
84.5% 15.5% |
|
Department Medical floors Surgical floors Orthopedic floors Maternity floor Pediatric floors Critical care units Emergency units |
112 125 49 59 65 105 97 |
18% 20% 8% 10% 11% 17% 16% |
|
Engagement in previous EBNP training/workshop Yes No |
427 185 |
69.8% 30.2% |
|
Engagement in previous nursing or health research Yes No |
155 457 |
25.3% 74.7% |
| Age (years) | Mean ± SD (31.86 ± 6.79) | |
| Years of experience | Mean ± SD (6.73 ± 2.39) | |
†SD, standard deviation, % percentage
Evidence-based implementation showed moderate significant correlation with facilitators, barriers, and competencies variables; having the strongest correlation with facilitators (r = .57, p < .01), followed by competencies (r = .48, p < .01) and barriers (r = - .39, p < .01). Weak significant correlations were found between belief variable and implementation (r = .38, p < .01) (See Table 2).
| No. | Variable/ variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | 1 | |||||||||||
| 2 | Gender | .13** | 1 | ||||||||||
| 3 | Education | .16** | -.02 | 1 | |||||||||
| 4 | Experience | .46** | -.02 | .22** | 1 | ||||||||
| 5 | Department | -.11** | -.09* | -.14** | -.12** | 1 | |||||||
| 6 | Workshop | .04 | -.12** | .28** | .07 | -.13** | 1 | ||||||
| 7 | Research | -.09* | -.12** | .13** | -.07 | -.09* | .08* | 1 | |||||
| 8 | Competency | -.04 | .01 | .22** | .13** | -.07 | .23** | .13** | 1 | ||||
| 9 | Beliefs | .05 | -.06 | .18** | .15** | -.01 | .23** | .13** | .16** | 1 | |||
| 10 | Facilitators | -.04 | -.05 | .26** | -.02 | -.07 | .24** | .15** | .48** | .11** | 1 | ||
| 11 | Barriers | .02 | -.04 | .01 | .03 | .02 | -.16** | .03 | -.35** | -.17** | -.39** | 1 | |
| 12 | Implementation | -.07 | -.06 | .15** | -.07 | -.04 | .37** | .32** | .48** | .38** | .57** | -.39** | 1 |
Testing the preliminarily hypothesized model
Preliminarily hypothesized model fit criteria (See Figure 2) showed a poor fit: (𝜒2/df = 2.892, p < .001, RMSEA = .063, GFI = .772, AGFI = .752, CFI = .871). After evaluating modification indices and parameter estimates, numerous paths were non-significant; subsequently, they were removed in order to make the measurement model more theoretically parsimonious. Likewise, age, gender, and department factors were removed.
Testing the modified stable model
The modified stable model presented in Figure 3 indicated improved fit indices than the preliminarily model: (χ2/df = 2.29, CFI = .94, RMSEA = .05, GFI = .90, AGFI = .88, CFI = .93).
Factors influencing implementation of evidence-based practice
The influencing factors on evidence-based practice implementation for nurses were specified (Table 3 and Figure 3). Explicitly, evidence-based practice implementation was significantly influenced by nurses' competency (𝛽 = .29, p < .001), beliefs (𝛽 = .27, p < .001), EBNP barriers (𝛽 = -.24, p < .001), and facilitators (𝛽 = .18, p < .001). The nurses' competency was most strongly related to evidence-based practice implementation. In total, the four factors explained 38.75% of the variance in evidence-based practice implementation.
| Outcome variables | Independent variables | β | Standardized effects | Squared multiple correlations | ||
|---|---|---|---|---|---|---|
| Direct effect | Indirect effect | Total effect | ||||
| Implementation | Competency | .29 | .29** | .14 | .43** | .39 |
| Beliefs | .27 | .27** | .05 | .33** | ||
| Barriers | -.24 | -.24** | -.24** | |||
| Facilitators | .18 | .18** | .18** | |||
| Barriers | Competency | -.31 | -.32** | -.01 | -.33** | .12 |
| Beliefs | -.11 | -.11* | -.11* | |||
| Facilitators | Beliefs | .16 | .16** | .16** | .05 | |
| Competency | .12 | .12** | .02 | .14** | ||
| Beliefs | Workshop | .18 | .18** | .02 | .20** | .10 |
| Competency | .12 | .12** | .12** | |||
| Research | .11 | .11* | .02 | .13** | ||
| Education | .09 | .09* | .02 | .11* | ||
| Experience | .08 | .08* | .02 | .10* | ||
| Competency | Workshop | .19 | .19** | .19** | .11 | |
| Education | .18 | .18** | .18** | |||
| Research | .10 | .10* | .10* | |||
| Experience | .10 | .10* | .10* | |||
The study findings show that nurses’ competency had a direct positive effect and indirect effect via nurses’ belief in evidence-based practice implementation. Similarly, beliefs had a direct positive effect and indirect effect via facilitators on evidence-based practice implementation. Greater barriers, in turn, predicted lower evidence-based practice implementation scores. In contrast, higher facilitators predicted higher evidence-based practice implementation scores. Both barriers and facilitators had only a direct effect on evidence-based practice implementation.
In addition, the influence of contextual factors (nurses' educational level, years of experience, attending EBNP workshops, and research conduction) on both nurses' competency and beliefs was examined. Nurses' competency was significantly influenced by attending evidence-based workshop (𝛽 = .19, p < .001), education level (𝛽 = .18, p < .001), years of experience (𝛽 = .10, p < .05), and previous research work (𝛽 = .10, p < .05). Attending evidence-based workshop was most strongly related to competency. Altogether, the four factors explained 10.9% of the variance in competency. Likewise, beliefs of the nurses was significantly influenced by attending evidence-based workshop (𝛽 = .18, p < .001), competency (𝛽 = .12, p < .001), previous research work (𝛽 = .11, p < .001), education level (𝛽 = .09 p < .05), and years of experience (𝛽 = .08, p < .05). Attending evidence-based workshop was most strongly related to beliefs. In total, these five factors explained 10.1% of the variance in competency (See Table 3).
Discussion
The study aimed to generate and validate a structural prediction model with the outcome of nurses’ implementation of evidence-based practice. The socio-demographic and personal profiles of the participants in this study were similar to those in previous studies exploring nurses’ competencies and beliefs regarding implementing evidence-based nursing practice within health care organizations (Hasheesh & AbuRuz, 2017; Verloo et al., 2017). Developing and validating a new conceptual model to assess multiple essential factors related to evidence-based practice implementation arose from the fact that most previous literature studied single or combinations of two or three factors without considering the sophisticated nature of evidence-based practice implementation (Squires et al., 2011; Cheng, Broome, et al., 2017).
The final model accounted for 39% of the variance of evidence-based practice implementation, which represented a large effect size (Cohen, 1992). However, a significant portion of variance remains undetermined, suggesting there are additional factors unaccounted for. Results of the current study confirm that the proposed model could be appropriate for this extended set of factors, as nurses’ competency, beliefs, facilitators, and barriers have a significant impact on nurses’ evidence-based practice implementation (See Figure 3).
In the modified stable model, competencies and beliefs of the nurses were the main predictors for nurses’ implementation of evidence-based practice. In addition, both factors were influenced by contextual factors, mainly the evidence-based workshops and training programs. Similarly, several researchers found significant positive associations of nurses’ competencies and beliefs with evidence-based practice implementation (Barako et al., 2012; Bostrom et al., 2013; Park et al., 2015; Cheng, Broome, et al., 2017; Alqahtani et al., 2020). Moreover, the current study indicated that nurses’ beliefs partially mediated the relationship between nurses’ competency and evidence-based practice implementation. Similarly, this result was congruent with a recent study conducted in KSA that found the same mediation effect (Alqahtani et al., 2020).
Other investigators found that the contextual factors (educational level, experience EBNP workshops or training program, and conducting research) were positively and significantly associated with the uptake of evidence-based practice (Barako et al., 2012; De Pedro Gomez et al., 2012; Farokhzadian et al., 2015; Hellier & Cline, 2016; Pereira et al., 2018). In addition, Alqahtani et al. (2020) found that both receiving evidence-based training and participation in research activity can influence the nurses’ knowledge. Moreover, Heydari et al. (2014) examined nurses’ competencies, beliefs, and implementation of evidence-based practice and found a significant positive correlation between educational levels and knowledge levels about evidence-based practice. However, Alqahtani et al. (2020) found that academic level was not associated with evidence-based implementation for Saudi nurses. This finding highlights the need to foster positive competencies and beliefs throughout providing in-hospital evidence-based practice training programs and workshops. Instilling competencies and beliefs in the benefit of evidence-based practice can be strengthened through multifaceted in-hospital evidence-based practice educational programs (van der Goot et al., 2018), which enable nurses to apply evidence-based practice knowledge and skills in practice (van der Goot et al., 2018).
An exciting finding from this study was the non-significant predictive effect of age, gender, and department in the proposed predictive model. This result was consistent with a recent Saudi study (Alqahtani et al., 2020). However, other studies found that increasing age, being female, and magnet status were found to positively and significantly impact evidence-based practice implementation scores (Hellier & Cline, 2016; Kim et al., 2016). This could be attributed to the variations in sample characteristics and settings. Although evidence-based practice competencies and beliefs were the chief predictors for nurses’ evidence-based implementation, barriers and facilitators also had a significant and direct impact on the outcome, thus highlighting the importance of the external organizational factors. Consistently, most studies about evidence-based practice discussed the impact of facilitators and barriers on the implementation of evidence-based practice (Johnston et al., 2016; Duncombe, 2018; Spooner et al., 2018; Lizarondo et al., 2019).
The current study presents the following limitations: (i) the results were taken from a convenient sample from various nationalities; there was probably a bias due to cultural diversities. Hence, the generalization of the results must be made carefully. Replication of the study with a larger, randomized sample in various regions and nursing settings is a necessity to increase the generalizability of the findings. (ii) Additional limitation was the use of self‐report questionnaires; thus, over-estimation of evidence-based competency, beliefs, and implementation is probable. Further research is recommended to include more factors like self-efficacy and confidence and their relation to nurses’ implementation of evidence-based practice.
Implications for Nursing Practice
The findings from the current study can lead the international efforts for nursing professionals to better comprehend the extent to which personal and organizational factors influence the implementation of evidence-based practice among registered nurses worldwide. The developed conceptual model may direct international future nursing research. Furthermore, this study implies that registered nurses need to improve their competencies, beliefs, and implementation of evidence-based practice. Also, the findings will help to lighten the hidden effects of organizational facilitators and barriers. Therefore, medical institutions, nursing front-runners, and policymakers might benefit from building up strategies and policies to promote registered nurses’ implementation of evidence-based practice through continuing education and mentoring programs about evidence-based practice.
In addition, national interventional programs should be developed and implemented to overcome the hidden organizational barriers and enhance evidence-based organizational facilitators. Decision-makers must place a high priority on the promotion of evidence-based practice if patients are to receive the best evidence-based care. This requires that evidence-based practice be tackled at the organizational as well as governmental levels if it is to be maintained.
Conclusion
The findings have highlighted the significant influence of nurses’ evidence-based competencies, beliefs, facilitators, barriers, and contextual factors toward nurses’ implementation of evidence-based practice. The developed model has the potential to support the transition of evidence-based practice competencies and beliefs to actual clinical behaviors; to meet professional necessities toward evidence-based practice; nevertheless, additional model validation is required. Further research is also advised to recognize other discipline-specific, personal, behavioral, and contextual factors that were not captured, as identified by the amount of model variance. Furthermore, this study presents the health authorities and nurses responsible for planning and providing evidence-based health services with insights into how to enhance evidence-based practice in KSA strategically. Therefore, interventions to increase the nurse’s competencies in evidence-based practice are needed. Educative training and in-hospital orientation programs that focus on the enhancement of competencies and health beliefs regarding evidence-based practice are required to promote the practice of evidence-based practice.