Background
Patients’ waiting time is defined as the quantity of time the patient devotes to waiting for services in a health facility (South Africa Department of Health, 2015). Although patients’ waiting time has been described as an important indicator in the determination of quality and efficiency of patient care, long waiting time remains a challenge in Primary Health Care (PHC) settings in several countries (Organisation for Economic Cooperation and Development (OECD), 2013). In this regard, long patients’ waiting times amount to delay in accessibility to health care services. In the United States of America (USA), the average patient waiting time ranges from 60 to 188 minutes (Tran et al., 2017). A study in Ethiopia revealed that 74 % of the patients’ waiting times ranged between 60 to 180 minutes (Belayneh et al., 2017). Additionally, in Nigeria, about a third (29.4%) of clients had to wait for three hours or more before they could be seen by a doctor (Akinyinka et al., 2016). The study in Mozambique revealed that patients queued for over one hour for registration, 180 minutes for outpatient consultation, and approximately two hours for first antenatal care visits (Wagenaar et al., 2016). In the South African context, despite the legal prescripts of several guiding frameworks, meaningful impact on lengthy patient waiting time remains difficult to achieve (Gauteng Department of Health, 2014; South Africa Department of Health, 2019). It is apparent that patient waiting time varies in different countries and settings.
Literature has demonstrated dire effects emanating from extensive patients’ waiting times in Community Health Centers (CHCs). In addition, the prolonged waiting time has been marked as a contributor to patients’ dissatisfaction (Motloba et al., 2018). The assertion is that patients have to withstand the discomfort of illness, at the same time, endure waiting to be served by health care professionals. As a result, missing appointments and moving from one facility to another demonstrates further hardships arising from prolonged patients’ waiting times (Egbujie et al., 2018). Other than that, lengthy waiting time persists as a challenge for nurse managers and staff alike (Egbujie et al., 2018). Dealing with dissatisfied and complaining queuing patients would be amongst a myriad of problems to be solved by nurse managers.
Certain interrelated dynamics related to the organization, healthcare workers, and patients have been allied with long waiting times. In support, Naiker et al. (2018) alluded that extreme patients’ waiting time may potentially be an indication of operational inadequacies in the CHC. Amicably, fewer healthcare providers would not be able to provide timeous efficient quality care to many patients, resulting in prolonged queuing. Furthermore, complex and tedious processes such as patients’ registration also prolong patients’ waiting time in clinics and CHCs (Viberg et al., 2013). Additionally, a lack of impactful policy direction has been linked to prolonged patients’ waiting time (Organisation for Economic Cooperation and Development (OECD), 2013). Therefore, it is imperative to get clarity from nurse managers regarding the compounding factors behind patients’ long waiting times.
Even though patients’ long waiting time has an immense effect on a multitude of stakeholders, the documentation has focused more on patients (Ward et al., 2017; Xie & Or, 2017). In the study conducted by Ward et al. (2017), patients experienced lesser psychological and physical well-being aftermaths. Furthermost South African studies concentrated on patients’ perspectives rather than managers and nurses. Accordingly, Munyewende and Nunu (2017) revealed that patients expressed discontentment regarding long waiting times. Conducting a study on views of managers as quality assurers would shed some light on understanding this phenomenon.
Despite the fact that patient waiting time is prioritized by National Core Standards, it remains a concern in CHCs Tshwane Health District (South Africa National Department of Health, 2016). The researcher, as a quality manager, observed that patients’ long waiting times at Tshwane health district CHCs still exceed the set target of less than 120-minutes (Gauteng Department of Health, 2017). Patients’ waiting time at these CHCs rose from an average of 168-minutes during the 2015/16 fiscal year to 209-minutes at the end of the 2017/18 financial year. That accounted for an increase in waiting times of 89-minutes. In addition, the volume of complaints serves as another performance indicator pointing to system inefficiencies. The number of complaints relating to long waiting times in the same period increased by 10% (Gauteng Department of Health, 2017). Based on the reviewed literature, there is a dearth of studies focusing on the views of CHC nurse managers regarding patients’ long waiting times. As a result, the purpose of this study was to describe and explore the views of nurse managers regarding patients’ long waiting times in CHCs in Gauteng Province.
Methods
Study Design
From March to November 2019, the research applied qualitative exploratory contextual design, which focused on real human experiences, meaning, and understanding from the point of view of managers in CHCs (Houser, 2018). Dense descriptions of data that emerged during the study enabled a better understanding of nurse managers’ views of patients’ long waiting times as accounting officers in charge of CHCs. Understanding the phenomenon of patients’ long waiting times is imperative in the era of COVID-19. The aftermath of the pandemic included, amongst others, many patients flocking to the health services, thus disrupting and overwhelming globally (World Health Organization, 2020). Waiting times could be one of the variables that are strongly affected by the current pandemic (Muschol & Gissel, 2021).
Participants
Purposive sampling method was championed in selecting a sample of eight nurse managers responsible for overseeing eight CHCs in the Tshwane District to explore and describe their views regarding patients’ long waiting times. According to the South Africa Department of Health (2009), the nurse manager is an operational manager who is appointed, delegated, or so assigned to manage the overall activities and personnel in a clinic or CHC. These nurse managers make an ideal target in this study as they were the administrative custodians solely responsible for discharging quality patient care, smooth running of CHCs, and dealing with all complaints regarding service delivery. Inclusion criteria were nurse managers working at Tshwane health district CHCs, with over a year’s experience.
Data Collection
The researcher was personally responsible for face-to-face data collection after obtaining permission from authorities. Appointments were made with participants, and then the researcher provided detailed information to the participants prior to obtaining their informed consent. All eight nurse managers agreed to participate in the study. Participants were allowed to volunteer and withdraw from the study at any time they deemed it necessary; however, none of them withdrew from the study. Semi-structured individual interviews were conducted in English at CHCs’ secluded noise-free areas identified by participants at their convenience. The interview guide comprised of two open-ended questions: 1) What are your views regarding patients’ long waiting time at CHCs? 2) What do you think can be done to reduce patients’ long waiting times at CHCs? Interviews that lasted for 64 to 105 minutes were captured with an audio recorder, and non–verbal cues were documented.
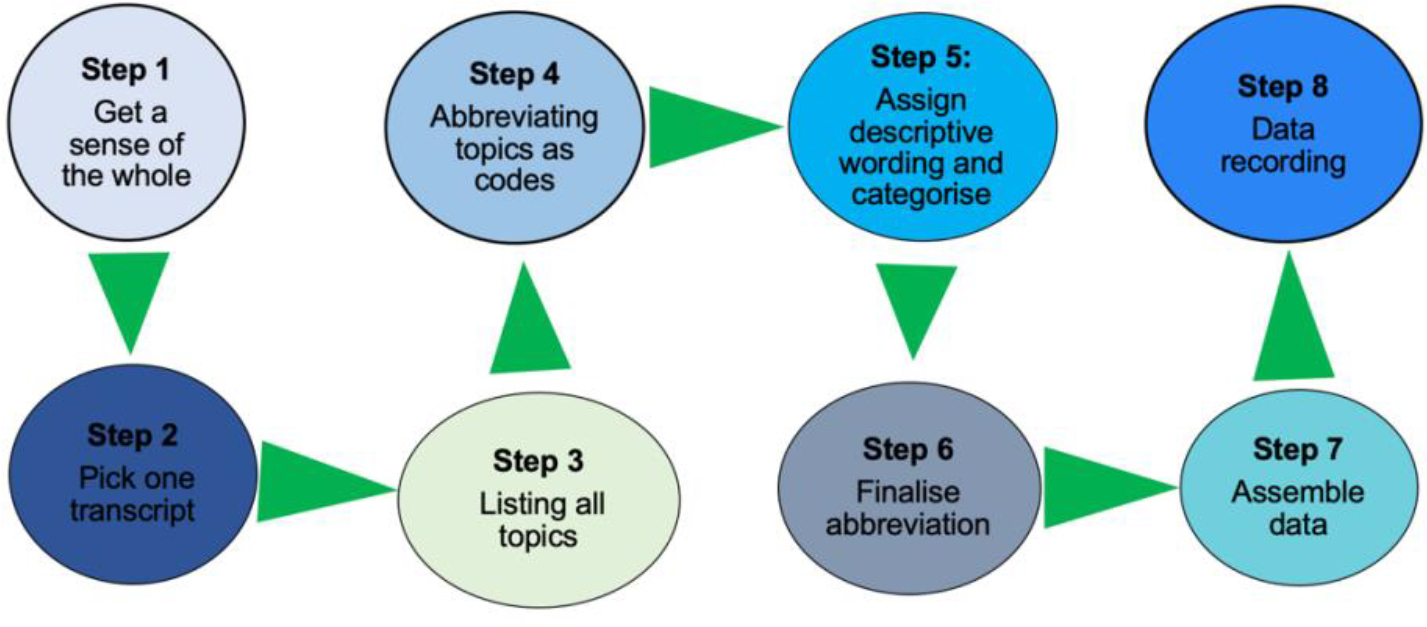
Data Analysis
Tesch’s eight steps of data analysis were followed to analyze data (Creswell, 2014). In the first step, the researcher read all transcripts and scripted down the emerging ideas to get a sense of the whole. This was followed by picking up transcripts one at a time, which were thoroughly read to get the emerging topics. These topics were then written down in the margin of the document. After reading all transcripts, a list of topics was compiled, which were compared to enable the grouping of similar ones. Fourthly, the main topics were highlighted and abbreviated with codes. These codes were duly indicated in the data in the appropriate sections. The fifth step involved assigning descriptive words to the identified topics as well as grouping them into categories. Subsequently, the researcher condensed these categories by deciding on the final abbreviation, including labeling each category and code to avoid duplication. The seventh step entailed grouping the data belonging to each category. The content of each category was analyzed to check whether they are relevant to the research question. The eighth step entailed data recording to get the whole meaning and general sense of data. This step was instrumental in enabling the blending of emerging topics into what was already analyzed. The data analysis process is summarized in Figure 1.
Trustworthiness
As guided by Korstjens and Moser (2018), trustworthiness is the degree to which typical characteristics of confidence, credibility, and authenticity manifest in qualitative research findings. The individual semi-structured interviews were recorded using an electronic audio recorder to seek the study’s credibility. This process enabled the researcher to capture all of the information adequately. At the same time, the field notes were captured in order to record the nonverbal cues displayed by the participants. Then, the follow-up was done whereby the transcripts were sent to all participants to be validated. Authentication of data was done by the qualitative researcher appointed as an independent co-coder and did not form part of the study. This was done to ensure confirmability. Credibility was ensured by immersion in the field until data saturation was achieved, thus aiding in gaining an in-depth understanding of the study phenomenon. The study was reviewed by two experts in quality patient care and PHC to fulfill the principle of dependability. Transferability was guaranteed through a robust description of study objectives, design, methods, and setting.
Ethical Considerations
The study obtained ethical clearance from UNISA’s Higher Degree Ethics Committee (Reference number: REC-012714-039). Permissions were also obtained from Tshwane Health District Research Committee. The researcher adhered to principles of respect, beneficence, and justice throughout the study (Polit & Beck, 2018). Participants’ rights were protected by obtaining both verbal and written consent prior to commencement. Confidentiality was guaranteed by reassuring participants that information shared would be inaccessible to any other unintended parties except those directly involved in the study. Codes, rather than participants’ names, were used to maintain anonymity.
Results
Characteristics of Participants
A total of eight CHC nurse managers participated in this study. Participants’ age ranged between 51 and 63 (Mean = 58.13 years; SD = 3.79). Majority of the participants were females (n = 7; 88%), married (n = 6; 75%). Five participants (63%) had four to ten years of experience in the current position. Three (38%) participants had a Bachelor of Nursing management followed by a Bachelor of Science in Nursing (n = 2; 25%) and a Diploma in Nursing Science and Midwifery (n = 2;25%), and Masters in Nursing Science (n = 1; 12%) (Table 1).
| Participants | Age (year) | Marital status | Gender | Education qualification | Experience in a managerial position |
|---|---|---|---|---|---|
| P1 | 53 | Married | Female | Bachelor of Nursing Science | 7 years |
| P2 | 61 | Single | Female | Diploma in Nursing Science and Midwifery | 5 years |
| P3 | 53 | Single | Female | Masters in Nursing Science | 7 years |
| P4 | 56 | Married | Male | Bachelor of Nursing Science | 4 years |
| P5 | 63 | Married | Female | Diploma in Nursing Science and Midwifery | 20 years |
| P6 | 60 | Married | Female | Bachelor of Nursing management | 13 years |
| P7 | 61 | Married | Female | Bachelor of Nursing management | 15 years |
| P8 | 58 | Married | Female | Bachelor of Nursing management | 10 years |
Study Results
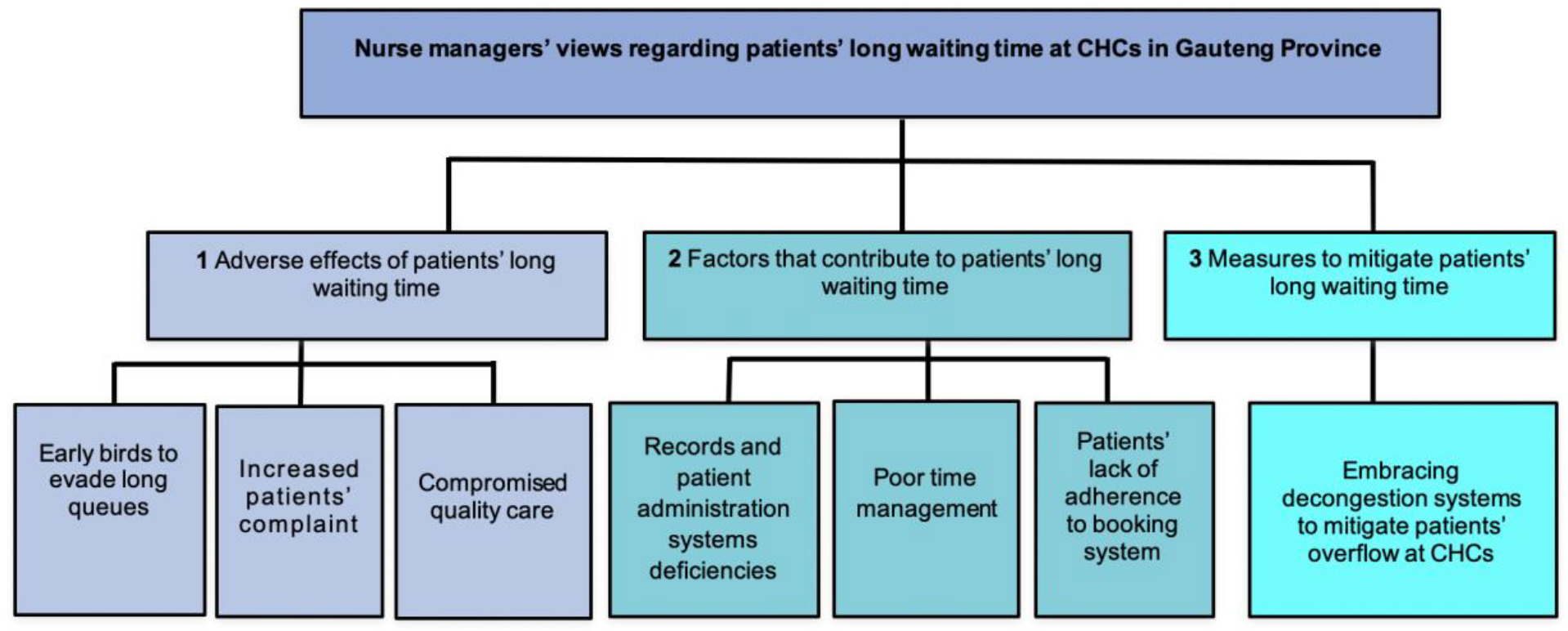
Dense descriptions of data that emerged during the study enabled a better understanding of nurse managers’ views of patients’ long waiting times as accounting officers in charge of CHCs. To that effect, three themes supported by seven categories emerged from the study (Figure 2). Each theme has categories described with the following direct quotes from the study participants.
Theme 1: Adverse effects of patients’ long waiting time
The majority of participants highlighted the adverse effects of patients’ long waiting time. This theme was supported by the following categories: Early birds to evade long queues, Compromised quality care, and Increased patients’ complaints.
Category 1.1: Early birds to evade long queues
On average, CHCs open their doors for day operations at 07h00. However, the experience as narrated by nurse managers has pointed to the prevalence of instances of arriving earlier than the normal day-time operating hours of the CHC. The following extracts bear testimony:
You see they come here as early as 03h00, and at that time, there is no one to monitor them. So, it has not yet become a problem for the facility per se, but should anything happen, while they are waiting, it will create or it’s going to expose us, yeah to say patients just come here and they wait for 07h30 (With a tense, worrisome expression). (P1)
They said they prefer to come earlier because now they want to be first, they can get services earlier in the morning. The others are staying in farms they are using the school bus; they said before school out, they must be finished so that they can go back earlier. (P7)
“Patients prefer to come earlier because now they want to be first… they can get services earlier in the morning. They come as early as 4 am…hey…(Sad looking) (P4)
Category 1.2: Increased patients’ complaints
Participants revealed lots of complaints from patients due to long waiting times. This is evident in the following citation:
Clients prefer to come to the office they don’t prefer to write. Every week or two, there must be complaints about the long waiting time. (P2)
The other way is the informal, through the informal complaint, and then you have the formal complaints where they actually use the complaint forms. In the worst-case scenario, they will report the facility to the presidential hotline or the Office of the Health Standards Compliance. (P1)
Clients prefer to come to the office they don’t prefer to write. Every week or two, there must be complaints about the long waiting time. Some of them are solved before coming to the office, but you will hear that there was a person complaining. (P3)
Category 1.3: Compromised quality care
Waiting time of the patient is an important determinant of the quality of the whole healthcare experience. Participants verbalized that due to long patients’ waiting times, they provided low-quality care to their patients. Participants verbalized a compromise in quality of care, as cited as follows:
Those who are in operations say they are not coping, and that leads to absenteeism that is chronic, quality of work is compromised, and they are just actually pushing the queue. (P7)
You need to understand that in June last year, we had a patient safety incident where a lady gave birth at the gate… (P1)
Theme 2: Factors that contribute to patients’ long waiting time
Participants mentioned several factors to long patients’ waiting times in the CHCs. These factors were described as follows: Records and patients administration systems deficiencies; poor time management and lack of adherence to booking system by patients
Category 2.1: Records and patient administration systems deficiencies
Study participants decried the competency and efficiency of current patient records and administration systems. Frustrated-looking participants narrated the following:
It creates a big problem. We have 70 000 patient files. The problem with it, we are unable to manage it. So, patients wait while one is looking for a file… (P8)
Risks exist that misfiling will be there. That one is unnegotiable. Remember, it’s a high volume of data with a limited number of people with ehh, improper filing cabinets, you know, everything is just not right, yeah. (P1)
Now we are using a new system which is Health Patient Registration System (HPRS), with 10 numbers, it does not bear any fruit… Three to four patients can have the same 4 numbers, so it is not up to scratch; it does not assist with anything. (P3)
Some other things that can really make a patient wait for a long time here are our system. The system that we are using is the HPRS system. Sometimes it is very much slow; sometimes, when it’s offline, you are unable to register the patient on the system. We have only one system, and then we see a lot of patients. (P8)
Category 2.2: Poor time management
Participants raised encounters of late coming, unauthorized meal-breaks extension, and early leaving by their staff.
I think one another thing again would be time management from staff, proper management of tea breaks, and lunch…(P2)
And I think they take long tea breaks as time for normal lunch, but rightfully tea break is just for stretching, having a cup of tea, and going back to work. (P6)
Another is common problem… our staff doesn’t relieve each other when they go for lunch or tea time. You find that there is nobody at the reception and patients are just waiting there… (P4)
Our clinicians who take their time to go and see patients, they are supposed to report on duty at 7 O’clock, but they start working at 9 O’clock, saying they are waiting for the files and they are not even encouraging admin staff to look for those files quickly. (P3)
Category 2.3: Patients’ lack of adherence to booking system
Participants experienced patient-oriented factors as influential in long waiting times at the CHC. In that regard, they highlighted two subcategories: lack of adherence to the booking system and patient overload. In addition, participants stipulated that patients also contributed to long waiting times at the CHCs. It emerged from this study that participants had experienced patients that do not honor their appointments as scheduled, thus impacting unfavorably on patients’ waiting time. As resonated as follows:
However, we have an uphill battle around that. Number one, we booked 350 patients, only 150 patients showed up, and now you have 200 patients not coming to the facility… The very same 200 will come tomorrow. (Angry facial expression). (P1)
But, for the mere fact that they don’t stick to that, we do our work, we pre-retrieve files, we book them, they don’t show up, wrong people come, now again we have to start from scratch to look for files to retrieve files, it’s not…not adding up. (P4)
Theme 3: Measures to mitigate patients’ long waiting time
Nurse managers have expressed measures that can reduce patients’ long waiting time. One category emerged as embracing decongestion systems to mitigate patients’ overflow at CHC.
Category 3.1: Embracing decongestion systems to mitigate patients’ overflow at CHC
This study’s participants pronounced on Centralized Chronic Medicines Dispensing and Distribution (CCMDD), treatment adherence clubs, and automated dispensing of medication as decongestion systems to mitigate patients’ long waiting time at CHCs. This is evident in the following citation:
Okay, the CCMDD is a system that the department brought in for chronic patients to be able to be seen once a year. And they just collect medication on a monthly basis, which makes it even easier, and it’s supposed to reduce the waiting time. (P5)
We know, studies have shown that it… you will never if… that is why even police stations and banks don’t use manual anymore, because you can’t be manual when you’re managing a high volume of data. The filing system must be digitized. (P7)
The filing system…, this is silly. We cannot always say, hide behind the budget. I mean, the budget will never be alright. If that was the case, we wouldn’t be having the Constitution of South Africa, because you wouldn’t say everyone will have the right to do that. The budget won’t allow, then we would actually have settled for a very poor constitution. (Throwing hands in the air) (P3)
Discussion
The study aimed to explore and describe the views of the nurse managers regarding patients’ waiting long times at the CHCs in the Tshwane Health District. The study revealed three themes: Adverse effects of patients’ long waiting time, Factors that contribute to patients’ long waiting time, and Measures to mitigate patients’ long waiting time. These themes are discovered as follows:
Adverse Effects of Patients’ Long Waiting Time
The majority of participants highlighted the negative experiences related to patients’ long waiting time. In this regard, the adverse effects of patients’ long waiting time, were supported by the following subcategories: Early birds to evade long queues, Economic impact, Compromised quality care, Increased patients’ complaints, and Violence against staff members.
Firstly, participants in this study expressed negative adverse effects of long patients’ waiting time as they observed that their clients reported very early at the CHCs. In their view, this strategy was employed by patients to that they could be attended to on the principle of first come first serve. Consistently, Kama (2017) found that patients queued around four o’clock in the morning just to afford them an opportunity to be in front of the long queues and avoid spending more waiting time. Caesar (2017) has further added that patients with appointments for later times during the day still arrive substantially earlier nonetheless. Early reporting could be related to the fact that patients resort to starting at CHCs so that they can attend other daily activities such as work or school. The strategy to report early at the CHCs, would also not assist patients because, under normal circumstances, most clinics’ routine operational activities start at seven o’clock in the morning. In this regard, queuing at CHCs without proper assessment and supervision can result in dire undiagnosed complications. Understandably, nurse managers as accounting officers should be concerned about this gesture.
Secondly, nurse managers narrated that they had to deal with a myriad of complaints from patients due to long waiting times. That could be related to patients’ dissatisfaction as a result of not being served on time. As substantiated by Xie and Or (2017), complaints over long patients’ waiting time could disrupt work patterns and processes in a facility. Hardine (2017) concurs in mentioning that being subjected to long waiting times invokes patients’ right to complain and demand recourse for the delays. The same nurse managers can’t just ignore these complaints but become beholden to investigate and redress as per complainant’s expectations thoroughly. Additional expression by Ganpisetti et al. (2018) exposed that patients’ complaints centered on the need to be promptly consulted, diagnosed, and further managed without undue delays. It is notable that nurse managers, in respect of their accountability, become entangled in the complaints as they need to resolve them (Ganpisetti et al., 2018).
Thirdly, participants verbalized that due to long patients’ waiting times, they provided low-quality care to their patients. Waiting time of patients is an important determinant of the quality of the whole healthcare experience. It is comprehensible that nurse managers were concerned about the low standard of care. A longer waiting time is likely to result in the patient experiencing more pains and complications. Examples provided by participants included unassisted pregnant women laboring in the queues. As similarly expressed by McIntyre and Ataguba (2014), some patients verbalized disappointment at the level of care rendered in the public hospitals, stressing amongst other contentions, long waiting hours before being attended to. Moscelli et al. (2018) added that bypassing facilities closer to patients’ abode has been associated with low quality of care and lengthy waiting periods. Gaynor et al. (2016) have emphasized that a considerable number of patients were more inclined to use hospitals with higher quality, even if it meant waiting longer.
Factors that Contribute to Patients’ Long Waiting Time
Participants mentioned several factors to long patients’ waiting times in the CHCs. These factors were described as follows: Records and patients administration systems deficiencies, Poor time management, and Lack of patient adherence to the booking system.
In this theme, the participants denounced the status of current patients’ records and administration systems. In this regard, the nurse managers highlighted that the ineffective disorganized filling system consequently contributed to patients’ long waiting time. Supportive findings by Marutha and Ngulube (2012) revealed that manual records management has not been assistive in improving services. Improper management of patients’ records would result in deferment in retrieving individual patients’ records, thus causing more delays. The ripple effect boils down to the awaiting patients in those registration areas. Mutale et al. (2013) added that these health system deficits delay performance optimization.
Participants raised a concern regarding poor time management amongst the staff as instrumental to long patient waiting time. Illustrations thereof include long breaks and reporting late for duty. Doctors were also blamed for poor time management. As a result, patients have to endure extra unused time just waiting for a late health care worker. In agreement, Almomani and AlSarheed (2016) reported that medical practitioners reported over forty minutes later than the expected time. Poor time management is, therefore, a call for concern as it is an aggressor towards lengthy waiting time.
Participants viewed patients’ conduct as synonymous with dishonoring their appointments, thus impacting unfavorably on waiting time. Failure to uphold an appointment would result in patients reporting to CHCs at any given period, thus overloading those scheduled for that particular day. A range of reasons has been captured from different studies as contributing to missed appointments. Frost et al. (2017) and Ramlucken and Sibiya (2018) advanced the following as primary reasons for missing their appointments: distance in reaching the facility, sudden ill-health, family responsibilities, dissatisfaction with facility services, and work obligations. Lack of adherence to appointment systems sabotages an effort of adequate planning and also causes a lot of inconvenience to CHCs. The CHC facility managers, in this regard, need to emphasize the prerogative role of patients through constant education.
Measures to Mitigate Patients’ Long Waiting Time
CHC nurse managers have expressed measures that can reduce patients’ long waiting time. One category emerged as embracing decongestion systems to mitigate patients’ overflow at CHC. Participants pronounced on Centralized Chronic Medicines Dispensing and Distribution (CCMDD) as decongestion coordination to diminish patients’ long waiting time at CHCs. In support, Ramphal (2019) applauded CCMDD, an alternative repeat treatment collection strategy for stable chronically ill patients. Following this process, patients will continue taking their treatment but not actually queueing for such at CHCs. Accordingly, automated dispensing systems save nurses time since all related logistics are handled by pharmaceutical companies themselves (Ahtiainen et al., 2020).
The Implications of this Study
Patents’ long waiting time is perceived as a problem amounting to a lack of access to health care services in South Africa and internationally. This phenomenon has dire implications for the international community when compounded with the aftermath of the global COVID-19 pandemic. The findings of this study show that nurse managers view the adverse effects of long waiting times. The nurse managers interpreted that patients report very early at the CHCs in order to evade the long waiting times. Nurse managers had to deal with a myriad of complaints from patients as a result of long waiting times. Additionally, quality patient care was compromised. Furthermore, according to the nurse managers’ views, several factors exacerbated patients’ long waiting times. For example, ineffective time management of the staff members delayed service delivery, thus elongating the waiting time. Deficiencies in records and patient’s administration resulted in long patient times. It was also noted that the implementation of decongestion systems is a necessity. The following recommendations emanated from the study findings:
Implementation of the appointment system should be optimized to avert long waiting times. In this regard, patients whose economic livelihoods are dented by missing work owing to spending all day at CHCs will reap the benefit of this effort. The appointment system should additionally be a platform to manage and prioritize patient over-load in the CHCs.
Amongst other interventions, prioritization of emergency, maternal, and child care, will help to prevent dire complications while dealing with long waiting times and appointment systems. Re-organization should continuously be re-evaluated to establish if it is yielding the intended results.
Collaboration between the CHCs’ management and clinic committees are important liaison structure between CHCs and local communities. They can both work together and team up to provide the best solutions to reduction of patients’ long waiting times. Clinic committees’ roles could be expanded to, amongst others, marketing, promoting, and advocating for the appointment system, assisting in resolving complaints as well as diffusing violence and abuse of staff by aggressive patients.
Time management is one area that needs to be improved on. Arriving and commencing duties on time, observing meal breaks, and knocking off at stipulated time should be normalized as corporate culture, such that transgressors castigate themselves with less effort from management. Perpetual deviations need to be consistently corrected. Where it needs to be, consequential and/or disciplinary actions should be instituted without hesitation. Nurse managers should oversee to it that time-wasters such as chit-chats and fruitless meetings are avoided.
Investing in electronic records and patient administration systems is yet another recommendation for the CHCs. These facilities consult large volumes of patients. The current traditional and manual management of records further compounds this. Going the digital route suffices to overhaul this experience. This should assist in resolving complaints of lost and misplaced files to eventually reduce the total time it takes to register just one patient.
Conduction of qualitative studies to explore how best to maximize operationalization of Batho Pele principles for frontline staff. Studies on a model to enhance collaboration in the reduction of patients’ long waiting time would provide solutions on how to deal with this matter and improve quality patient care.
Limitations of the Study
The study employed a qualitative design in one province, thus rendering it difficult to generalize the findings to other CHCs in and outside South African borders.
Conclusion
Participants highlighted the adverse effects of patients’ long waiting time in CHCs. It was clear that due to long waiting times, patients reported very early at CHCs. In addition, quality patient care was compromised in that the service provided was rushed in order to serve as many patients as possible. Due to long waiting times, participants had to deal with complaints from patients. Factors such as poor filing system was blamed for patients’ long waiting times. Participants also pointed out that poor punctuality amongst health care workers contributed to prolonged patients’ waiting time. In addition, lack of adherence to the appointment system by patients was found to contribute to long waiting times in that they would all come to CHCs simultaneously. Participants emphasized the need to embrace decongestion systems such as CCMDD to diminish patients’ long waiting time at CHCs.