Readmission among myocardial infarction (MI) patients (MIPs) has become the principal marker of the quality of care (Dunlay et al., 2012; Kwok et al., 2018). Despite improvements in acute care and survival after hospitalization, readmission remains an important contributor to health care costs (O'brien et al., 2017; Southern et al., 2014). A previous study found that 62% of MIPs are readmitted within one year (Southern et al., 2014). There are several reasons for readmission, such as poor adherence to advice for health (i.e., adhere to medicine, nutrition, and restricted fluids), emotional or mental factors (i.e., mood status, substance abuse, and impairs the cognitive function), environment, insufficient discharge program, and other health problems (Annema et al., 2009; Jenghua & Jedsadayanmata, 2011; Ryan et al., 2014). Thus, readmission remains a significant health problem, a frequent, high cost of care, and a life-threatening event, as well as it is related to the quality of care (Hasan et al., 2010; Jencks et al., 2009).
In Thailand, MI is a leading cause of death, from 2014 to 2018 (Charupronprasit et al., 2017). However, there is very little information on readmission among MIPs. Although a previous study found that the rate of readmission of MIPs was 14.07%, caused by chest pain and chronic kidney failure (Jenghua & Jedsadayanmata, 2011), it is impossible to draw a reliable conclusion from this finding. In addition, an abundance of research documents on readmission have been conducted in the United States (USA), where factors related to readmission have been reported, but may not entirely apply to Thailand (Coffey et al., 2012; Hasan et al., 2010; Polsook et al., 2013, 2016).
Numerous interventions have successfully reduced readmission rates among MIPs, such as discharge programs, advising and counseling programs, and medication regimen programs (Annema et al., 2009; Jenghua & Jedsadayanmata, 2011; Ryan et al., 2014). However, the percentage of readmission in MIPs is continue to rise. In Thailand, little investigation has been carried out on the factors related to readmission among MIPs. Since characteristics of Thai’s culture are incompatible with the USA, it is logical to suspect that findings of research in the USA may partially differ from the situation in Thailand because of the different cultural characteristics, such as income and education, which were reported to be connected to readmission (Annema et al., 2009; Coffey et al., 2012; Hasan et al., 2010; Jencks et al., 2009).
As the biggest health care professionals’ group, nurses contribute in a positive and negative way to the problem of health care quality. Nurses have an intimate understanding of patient needs and important roles in caring for patients and family, and uniquely position them to positively affect their hospital experiences and subsequent outcomes (Duffy, 2009, p. 6). The quality of care is a model designed to support the understanding of the connection between quality health care and caring (Duffy, 2009, p. 35). This model is composed of three elements of a quality caring model (Duffy, 2009). The structure is the first element, which consists of the resources of the institution, provider credentials, and characteristics of the patient. This paper focused on the characteristic of the patients because we were required to emphasize the independent variables associated with the patients. The process is the second element, which refers to the actions done for the patient, including both the practical and relational aspects of care. The outcomes are the third element, which refers to the consequences of the health care process (Duffy, 2009; Polsook & Aungsuroch, 2020). This study focuses on the characters of MIPs, because we aimed to maneuver the variables associated with the patients beforehand, emerging a procedure to enhance the result of care (Polsook & Aungsuroch, 2020).
The pursuing variables linked to readmission in MIPs have been recorded. These factors are social support, depression, comorbidities, symptom severity, and quality of life (QOL) (Annema et al., 2009; Polsook & Aungsuroch, 2020). The connection amongst variables can be illustrated as follow: (1) social support is a significant predictor of QOL and high level of social support relevant to the high quality of life resulting in decreased readmission in MI (Bennett et al., 2001; Volz et al., 2011); (2) depression is negatively associated to QOL and linked to readmission (Faller et al., 2010; Heo et al., 2009); (3) symptom severity has a strong association with QOL, with higher severity of symptoms related low QOL and frequency readmission (Faller et al., 2010; Giamouzis et al., 2011); (4) comorbidity is a significant predictor of readmission and comorbidity is a disease and overload connected with rising readmission (Benbassat & Taragin, 2000; Hasan et al., 2010; Kansagara et al., 2011); and (5) patients who have experiences with physical and emotional symptoms result in reduced QOL, which is connected to the higher incidence of readmission (O'loughlin et al., 2010; Sethares & Elliott, 2004). Given the linkage of the variables on readmission, this study aimed to test a model to explain how those potential factors influenced readmission in Thai MIPs.
Methods
Study Design
This research employed a descriptive cross-sectional design.
Sample and Setting
The population in this research was Thais with myocardial infarction. A total of 200 MIPs were recruited from excellence center hospitals across Thailand. The sample size was derived from Hair et al. (2010), which at least 200 samples recommended for a complex model with more constructs. Additionally, the adequate sample size for path analysis is ten times for each parameter. This research had 13 parameters; thus, a sample size of 130-260 was the requirement to match the complexity to the path model.
A modified multi-stage sampling method was used to select the samples from hospitals based in the Northern, Southern, Central, and Northeastern regions of Thailand. The inclusion criteria were: (i) recently readmitted in an inpatient cardiology department in one of five selected hospitals in Thailand, (ii) aged ≥ 20 years, and (iii) having no cognitive impairment or disease complications based on their current medical record. If the participants had any exacerbations of the disease, such as shock, acute pulmonary edema, acute shortness of breath, and acute chest pain, during collecting data were excluded.
Instruments
The questionnaire on sociodemographic characteristics was designed to gather sociodemographic data, including gender, age, marital status, type of health care coverage, readmission, comorbidity, and symptom severity (Polsook & Aungsuroch, 2020). Readmission refers to the number of MIPs repeatedly hospitalized within 12 months of discharge from the index hospitalization collected from their medical records (Polsook & Aungsuroch, 2020). Comorbidity refers to the presence of additional conditions co-occurring with MIPs and was collected from the medical record (Polsook & Aungsuroch, 2020).
The severity of symptoms was used in the Canadian Cardiac Society (CCS) classification to categorize angina pectoris, including Class I – angina pectoris during intensive or long-term physical activity, Class II – angina pectoris with moderate exertion, Class III – undergoing angina with mild exertion, and Class IV – undergoing angina at rest (Polsook & Aungsuroch, 2020; Sangareddi et al., 2004).
Multidimensional Scale of Perceived Social Support (MESSI) (Zimet et al., 1988) was used to measure social support. This scale was translated into a Thai version by Wongpakaran and Wongpakaran (2012). The scale consists of 12 items to evaluate perceived social support from friends, family, and significant others. A seven-point (1–7) Likert scale was used, ranging from 1 to 7, with a total score for 12 items of 12–84. A higher rating is an indication of a higher level of social support. Cronbach’s alpha coefficient was 0.89 (Phromsornt et al., 2019; Polsook & Aungsuroch, 2020).
Cardiac Depression Scale (CDS) was used to measure depression. The scale consists of 26 items to measure sleep, uncertainty, mood, hopelessness, inactivity, anhedonia, and cognition (Hare & Davis, 1996; Oldridge, 1997). This scale was translated into a Thai version by Polsook and Aungsuroch (2019). The CDS uses a 7-point scale from 1 to 7, with a score excess of 100 is delineated as strong depression (Kiropoulos et al., 2012). Cronbach’s alpha coefficient of the Thai version was 0.82 (Polsook & Aungsuroch, 2019).
Quality of life Index-Cardiac version IV Thai version (QLI-cardiac IV) was translated into a Thai version by Saengsiri and Hacker (2015): The QLI-cardiac IV was developed to assess the QOL regarding the life’s satisfaction of cardiovascular patients. This instrument includes about 70 items to measure the satisfaction of patients with several aspects of life (35 items) and assessed the importance of those same aspects (35 items). The scale used on a 5-point scale ranging from 0 to 5 and a final rating scale ranging from 0 to 30. A rating between 21 and 30 is described as a high QOL. Cronbach’s alpha coefficient of the Thai version was 0.91 (Polsook & Aungsuroch, 2019; Saengsiri & Hacker, 2015).
Data Collection
Data collection was carried out after the approval of each hospital's Institutional Review Board (IRB) was obtained. The researcher illuminated and clarified the study objectives, data collection procedures, expected outcomes, and the study’s benefits to the physicians and nurses of each cardiology inpatient department in the chosen hospitals. One nurse with experience in taking care of cardiovascular patients was assigned as a research assistant. The researcher trained and evaluated the research assistants in regards to the questionnaire administration, informed consent procedures, and the participant information sheet. Research assistants were also trained to interview the participants by reading the questionnaires word by word.
Participants who met the inclusion criteria were then invited to participate in this study. They were informed of the study objective, data collection process, and their rights to decide to participate or refuse to participate in the study. Those participants who still agreed to participate in this study were asked to sign an informed consent form. The researcher explained that there was no harm to the participants in this study and that it would take 30–45 min to complete all the questionnaires. During data collection, participants were able to refuse or leave the study at any time without any consequence (Polsook & Aungsuroch, 2020).
Data Analysis
The Statistical Package for Social Science (SPSS) program version 22 was used for data analysis, particularly in descriptive statistics. Linear Structural Relationship (LISREL) version 8.72 was used for path analysis, accepting significance at the p < 0.05 level. The statistical criteria by Hair et al. (2010) were used to evaluate the overall model-fit-index and the hypothesis according to the four criteria outlined as follows. Firstly, the χ2 test was used to evaluate the appropriateness of the hypothesized model. The model was considered a good fit if the χ2 value was not significant (p > 0.05) and if χ2 /df was less than 2. Secondly, the Root Mean Square Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR) were used to measure the overall model fit. RMSEA value of less than 0.05 was considered a good fit model, while a value between 0.05–0.08 was considered an adequate fit model. In addition, the SRMR value should be less than 0.05 for a good fit model. Thirdly, a goodness-of-fit (GFI) ≥ 0.95 and adjusted GFI (AGFI) ≥ 0.90, were also used for examining the goodness-of-fit statistics. Finally, if the hypothesized model fit the data, the path coefficients and R2 were then estimated, and the effects of the independent variables on the dependent variable were determined. The goodness-fit-indices were used to determine whether the model adequately fitted the data (Hair et al., 2010)
Ethical Consideration
This study was approved by the IRBs of the excellence center care hospitals from all regions of Thailand. Those IRBs included the IRB of Hatyai hospital (Approval Number 85), the IRB on Human Right Related to Research Involving Human Subjects of the Faculty of Medicine Ramathibodi Hospital Mahidol University (Approval Number 2558/716), IRB of the Faculty of Medicine Chiang Mai University (Approval Number 2558-03518), IRB of the Faculty of Medicine Chulalongkorn University (Approval Number 074/59), and IRB of Khon Kaen University (Approval Number 00001189) (Polsook & Aungsuroch, 2020).
Results
Characteristics of Participants
Most of the participants were aged ≥ 61 years (62.5%), predominantly male (63%), and married (78.5%). Just over half of the participants (54.5%) utilized the Universal Coverage Scheme (the 30-Baht Scheme) of Thailand. The highest proportion of participants with an education level was primary school (52.0 %), followed by high school (24.5%), and higher education (19.5%). According to the classification of symptom severity by the CCSV (Sangareddi et al., 2004), 28.5% of the participants were in class 1, 33% in class II, 19.5% in class III, and 19% in class IV. The majority of participants had one (40.5%) or no (24.5%) comorbidity. In addition, most of them (88%) were readmitted only 1 or 2 times within 12 months after the initial hospital discharge is shown in Table 1. Details about each variable's characteristics are presented in Table 2.
| Characteristics | Number (n) | Percent (%) |
|---|---|---|
| Age | ||
| 20–40 | 10 | 5 |
| 41–60 | 65 | 32.5 |
| ≥ 61 | 125 | 62.5 |
| Gender | ||
| Male | 126 | 63 |
| Female | 74 | 37 |
| Marital status | ||
| Single | 10 | 5 |
| Married | 157 | 78.5 |
| Widowed | 28 | 14 |
| Divorced | 5 | 2.5 |
| Education level | ||
| Non-education | 8 | 4 |
| Primary school | 104 | 52 |
| High school | 49 | 24.5 |
| Higher education | 39 | 19.5 |
| Type of health care coverage | ||
| Universal Coverage Scheme (30-Baht Scheme) | 109 | 54.5 |
| Social security | 12 | 6 |
| Pay by themselves | 5 | 2.5 |
| Government coverage | 74 | 37 |
| Canadian Cardiovascular Society Classification | ||
| Class 1 | 57 | 28.5 |
| Class 2 | 66 | 33 |
| Class 3 | 39 | 19.5 |
| Class 4 | 38 | 19 |
| Comorbidities | ||
| No comorbidity | 49 | 24.5 |
| One comorbidity | 81 | 40.5 |
| Two comorbidities | 37 | 18.5 |
| Three comorbidities | 33 | 16.5 |
| Readmission (within 12 months of discharge from hospital) | ||
| 1–2 times | 176 | 88 |
| 3–4 times | 20 | 10 |
| 5–6 times | 2 | 1 |
| 7–8 times | 0 | 0 |
| 9–10 times | 2 | 1 |
| Variable | Mean | Standard deviation | Interpretation |
|---|---|---|---|
| Readmission | 1.16 | 0.53 | 1–2 times |
| Social support | 64.03 | 13.66 | High |
| Depression | 86.34 | 26.27 | Not depressed |
| Quality of life | 24.66 | 2.94 | High |
| Comorbidity | 2.27 | 1.01 | One comorbidity |
| Symptom severity | 2.30 | 1.08 | Class II |
Relationships Between Variables
The relationships among the social support, depression, symptom severity, comorbidity, QOL, and readmission were examined using the Bivariate Pearson’s correlations (Table 3), with the extent of the relationships defined by the following criteria: r > 0.50 = strong / high relationship, 0.30 ≥ r ≤ 0.50 = moderate relationship, and r < 0.30 = weak/low relationship (Burns & Grove, 2005). The social support had a low negative correlation with readmission (r = -0.06, p < 0.05), depression and symptom severity had a low positive correlation with readmission (r = 0.11, and r = 0.10, p < 0.05), and no correlation was found between readmission and comorbidity and QOL (r = 0.00 and r = 0.00, p < 0.05). Depression, symptom severity, and comorbidity all had a low negative relationship with the social support (r = -0.16, -0.04, and -0.05, respectively; p < 0.05). The QOL had a low positive relationship with social support (r = 0.25, p < 0.05) and a moderate negative correlation with depression (r = -0.39, p < 0.05), a low negative correlation with comorbidity (r = -0.15, p < 0.05) and symptom severity (r = -0.18, p < 0.05). The symptom severity had moderate positive correlation with depression (r = 0.36, p < 0.05), while comorbidity had a weak positive correlation with depression (r = 0.13, p < 0.05) and symptom severity (r = 0.20, p < 0.05).
Model Testing
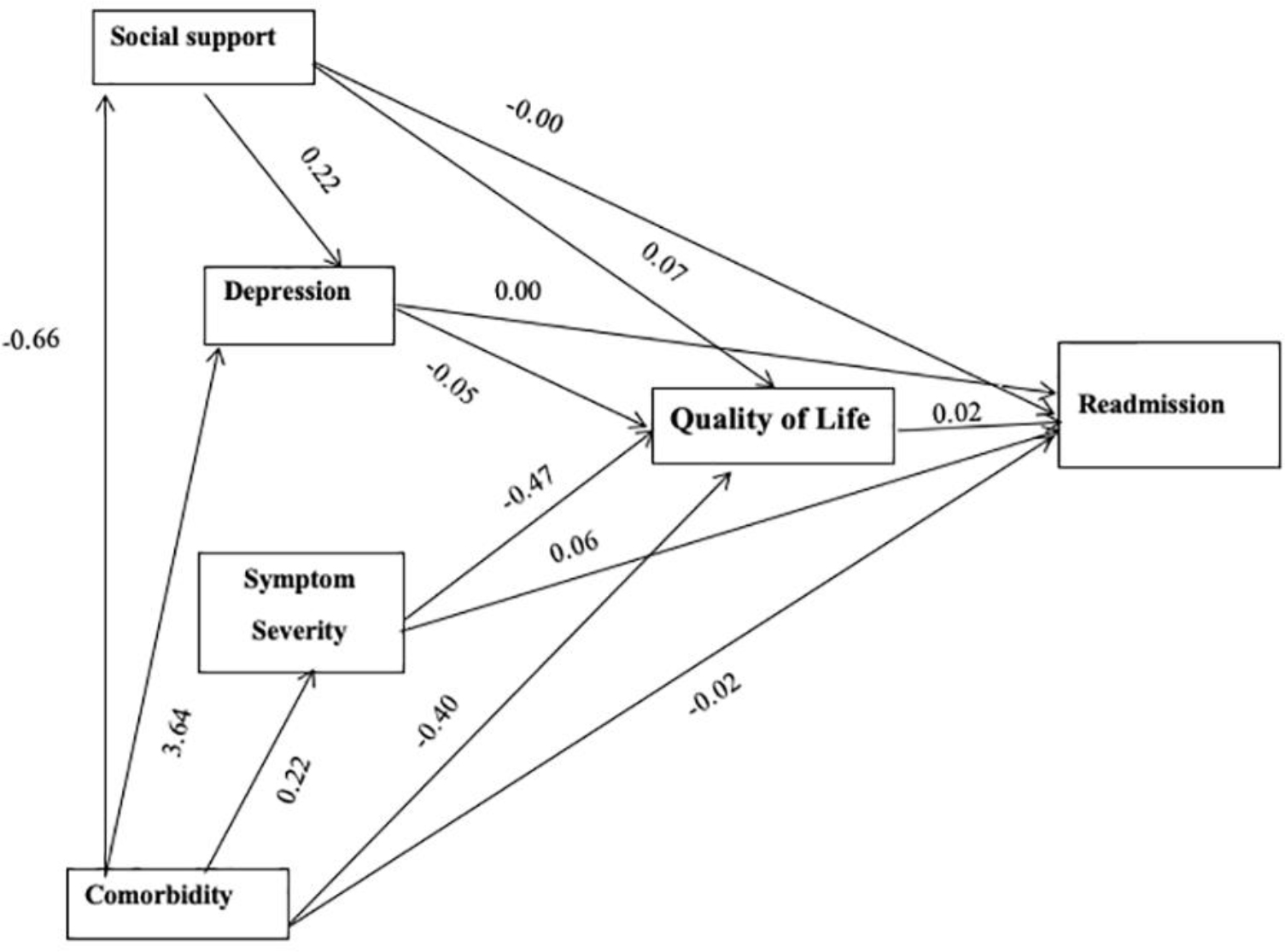
The results from the hypothetical pattern matched the empirical evidence and could explain 4% (R2 = 0.04) of the variance in readmission by social support, depression, symptom severity, comorbidity and QOL (χ2 = 1.39, df = 2, p = 0.50, χ2/df = 0.69, GIF = 1.00, RMSEA = 0.00, SRMR = 0.01, and AGFI = 0.98). Twenty-eight percent (R2 = 0.28) of the variance in the QOL was explained by the social support, comorbidity, symptom severity, and depression; 3% (R2 =0.03) of the variance in depression was explained by social support, comorbidity, and symptom severity; and 4% (R2 =0.04) of the variance in symptom severity was explained by comorbidity (Table 4).
| Variables | Influencing variables | R2 |
|---|---|---|
| Readmission | Social support | |
| Comorbidity | ||
| Symptom severity | 0.04 | |
| Depression | ||
| Quality of life | ||
| Quality of life | Social support | |
| Comorbidity | 0.28 | |
| Symptom severity | ||
| Depression | ||
| Depression | Social support | |
| Comorbidity | 0.03 | |
| Symptom severity | ||
| Symptom severity | Comorbidity | 0.04 |
R2 = The coefficient of determination
The results of the final model testing as shown in Figure 1 are summarized in accordance with the hypothesized model as follows. The QOL had a direct positive impact (0.02) on readmission, while social support and depression did not directly affect readmission (0.00, 0.00). Besides, symptom severity had a direct positive impact (0.06) on readmission, contrasting with comorbidity that had a direct negative impact (-0.02) on readmission. Social support had a positive direct effect (0.06) on QOL and a negative effect (-0.01) through QOL on readmission. Comorbidity had a direct negative impact (-0.40) on QOL and a negative effect (-0.27) through QOL on readmission. Symptom severity had a negative effect (-0.47) on QOL and had a negative effect (-0.01) through QOL on readmission. Depression had a negative effect (-0.05) on QOL, while social support had a positive effect (0.22) on depression. Besides, comorbidity had a positive effect (3.64) on depression. It also had a positive effect (0.22) on symptom severity and a negative effect (-0.66) on social support.
Discussion
This study revealed that social support did not affect the readmission of MIPs. Most of the participants were elderly, and their social support was at a moderate level. Because Thailand had an extended family, most participants live with their families, where there is a possibility that family members may have been involved in the patient's care and support (Polsook et al., 2013, 2016). This finding was supported by Leifheit-Limson et al. (2012), who reported that a high social support level was associated with lower hospital readmission of MIPs. Similarly, Mcneely et al. (2016) found that high social support in MIPs who received the percutaneous coronary intervention was associated with a lower rehospitalization rate.
Additionally, we found that social support had a direct positive impact on depression, where most of the MIPs in this study had a high social support level living with their extended family and were not depressed. Leifheit-Limson et al. (2012) found that a low social support level was related to more depressive symptoms among MIPs, and a high social support level resulted in a low level of depression. It is supported by Compare et al. (2013) and Liu et al. (2017) reported that an elevated level of social support lowered depressive symptoms among heart patients.
This study also found that social support had a positive impact on the QOL and a negative indirect impact on readmission through the QOL. Since most participants had an elevated QOL and social support level, they were only readmitted one or two times within the 12 months after initial hospital discharge. This result supported previous studies in that social support had a positive impact on the QOL among MIPs (Kang et al., 2018). In addition, the QOL, an outcome measurement after acute MI, was lower in the early recovery period when there was an inadequate social support level (Leifheit-Limson et al., 2012). Likewise, a high social support level in MIPs was linked to a high QOL and reduced readmission (Martínez-García et al., 2018).
In this study, depression was not an effect on readmission, a negative indirect effect on readmission through the QOL, and a negative direct impact on the QOL. This reflected that most of the MIPs were not depressive, having a high QOL and low readmission rate of only one–two times within the 12 months after initial hospital discharge. In agreement, a high level of depression was reported to be related to hospital readmission and a decreased QOL (Kang et al., 2018), while depression was also associated with readmission in acute coronary syndrome (Edmondson et al., 2014).
The symptom severity was found to have a negative direct impact on the QOL and a positive direct effect on readmission. As already pointed out, most of the MIPs in this study had a high QOL and symptom severity of only class I (28.5 %) or class II (33%) of the CCSC, which their low symptom severity resulted in a high QOL and reduced readmission rate. This result supported previous studies that low symptom severity was linked to delayed readmission (Kwok et al., 2018) and an increased QOL (Kang et al., 2018) among acute MIPs. Likewise, the symptom severity, such as physical symptoms and limitations in daily activities due to heart failure, affected the QOL (Heo et al., 2009). Low symptom severity was linked to a higher QOL (Adebayo et al., 2017).
In our study, nearly half of the participants had one comorbidity. About one-third had no comorbidity, no depression, a high QOL, and a low readmission rate (one or two times within 12 months after hospital discharge). Thus, the participants’ low comorbidity was related to their low level of depression, which resulted in a high QOL and a low readmission rate. In agreement, MIPs who received a percutaneous coronary intervention had a high rate of readmission if they had comorbidity (Kwok et al., 2018; Southern et al., 2014), while the presence of more comorbidities had a higher risk of hospital readmission (Andrés et al., 2012; Kwok et al., 2017), as well as high symptom severity and readmission risk (Desta et al., 2017; Fanari et al., 2017; Mcneely et al., 2016). In addition, MIPs who had comorbidity were associated with depression and linked to readmission (Mcgowan et al., 2004).
The results also revealed that lower comorbidity led to lower symptom severity and high QOL. These results are also in line with a previous study (Bahall & Khan, 2018), while a low symptom severity, such as shortness of breath and chest pain, related to a high QOL in heart failure patients (Lawson et al., 2018; Nuraeni et al., 2019). Besides, QOL has been shown to directly impact the readmission rate, which a high QOL was associated with a low rate of readmission. Previous studies found that a poor QOL led to a higher rehospitalization rate and was associated with readmission (Adebayo et al., 2017; Tully et al., 2016).
This study has several limitations. The self-reporting used in this study might cause overvalued or undervalued data, which could be a limitation. The instruments to measure the potential variables were only used once in the context of Thailand. Thus, assessing validity and reliability within Thailand's context is required to confirm the instruments' reliability. Based on the findings of this study, a longitudinal study should be done to measure and adjust these variables with readmission in MIPs to provide a further causal explanation of readmission in MIPs and its predictors. However, our findings can contribute to knowledge development for strengthening nursing science for caring MIPs. The results provide knowledge that offers directions for the development of interventions to decrease readmission in MIPs. It should promote social support to enhance the QOL and develop strategies to control the severity of symptoms to mitigate readmission in MIPs.
Conclusion
Based on these findings, the severity of the symptoms and QOL of MIPs were correlated to readmission. Nurses should develop strategies to control or decrease symptom severity and develop an intervention protocol to reduce readmission in MIPs. This should integrate the promotion of social support to enhance the QOL to decrease readmission and increase care quality for MIPs.