Background
Cold or warm water was used in labor processes for maternal relaxation and anesthesia for a long time. Water birth started in the 18th century as hydrotherapy. It was used by Egyptian, Roman, and Greek physicians (Brooks, 2018). The first water birth was conducted in France in 1805. Few physicians claimed that a woman with prolonged labor (almost 48 hours) gave her birth immediately after water submerging. In 1960, a gynecologist from Russia detected the impact of water birth on improving newborn findings. Later, a researcher reported his intervention with 100 water births. He advocated that there was no risk associated with water birth and that water immersion reduced the need for interventions and analgesia during labor (Lim et al., 2016). In this regard, 150,000 water deliveries were done between 1985 and 1999, according to Rosales et al. (2017).
In India, the first water birth was conducted in 2007; however, it was not recommended because of the lack of skills and safety for the mother and her newborn (Dular & Jyoti, 2019). Nevertheless, in several parts of the world, the water delivery rate during labor is remarkably growing (Darsareh et al., 2018).
Water birth involves complete immersion of the mother’s abdomen in a pool of water that allows her to change her position freely during labor (Darsareh et al., 2018). Various positions can be used underwater, such as squatting, kneeling, and sitting while putting a head on a pillow while resting on the side of the pool. In addition, pregnant women can be immersed in warm water when their cervix is dilated by around 5 cm (Dular & Jyoti, 2019). There are criteria for pregnant women to have a safe water birth as gestational age of above 37 weeks, singleton pregnancy, normal labor, vertex presentation, normal blood pressure, normal fetus, and clear amniotic fluid. In contrast, contraindications for water birth are BMI of more than 25, medical health problems, unstable fetal heart rate, intrauterine growth retardation (IUGR), antepartum hemorrhage, herpes simplex infection, and administration of pethidine analgesia in labor (Dular & Jyoti, 2019).
Water birth has been considered an efficient non-pharmacological modality with numerous maternal and neonatal benefits. Regarding the maternal benefits, water birth increased maternal satisfaction and reduced the sensation of heaviness and pain during labor (Brooks, 2018; Cooper & Warland, 2019; Reyhan, 2019). In addition, according to a previous study, water birth increased maternal comfort during childbirth and decreased stress and anxiety (Brooks, 2018; Walls, 2017).
Furthermore, other studies reported reasons to choose water birth as a delivery method, including being non-pharmacological or natural, increased maternal focus, and control during labor (Brooks, 2018; Cooper & Warland, 2019). Moreover, water birth has an analgesic effect, reducing the need for epidural analgesia (Brooks, 2018). Further, water birth decreases the rate of perineal laceration, cesarean section delivery, and prolonged second and third stages of labor, as well as the need for medical interventions such as episiotomy (Brooks, 2018; Kavosi et al., 2015; Szymkowiak et al., 2017). In this regard, women who had water birth expressed the feeling of safety, protection, and security and recommended water birth for others (Akhlaghi et al., 2017; Cooper & Warland, 2019). Physiologically, water birth has been reported to increase endorphin level and pelvic diameter and decrease blood pressure and the duration of the first and second stages of labor (Brooks, 2018; Dular & Jyoti, 2019; Walls, 2017). Moreover, it improves uterine perfusion and labor progress. Also, it decreases catecholamine, stretches the vagina, and facilitates the delivery of the fetus (Dykes, 2017). Further, it increases the elasticity of the perineum, oxygen, blood supply to the fetus, and endogenous oxytocin production (Brooks, 2018; Cooper & Warland, 2019; Kavosi et al., 2015).
Regarding neonatal effects, there is no evidence of increased complications associated with water birth, in addition to the rarely reported side effects (Lim et al., 2016). On the other hand, water birth has been reported to improve bonding and skin-to-skin contact, according to Walls (2017), decrease the risk of respiratory distress syndrome and hypoxia, as reported by Szymkowiak et al. (2017) and regulate body temperature (Darsareh et al., 2018; Dykes, 2017).
Findings of previous studies suggested that water birth has non-significant maternal or neonatal complications. However, water aspirations, postpartum hemorrhage, severe stages of perineal tears, maternal or newborn infection, and retained placenta were observed among some water birth parturients (Brooks, 2018; Cooper & Warland, 2019; Lim et al., 2016). In this regard, attention should be paid to the risk of umbilical cord avulsion at water births (Ulfsdottir et al., 2018). On the other hand, another study showed no maternal or neonatal complications related to water birth (de Camargo et al., 2022; Dykes, 2017; Reyhan, 2019; Walls, 2017). Further, a retrospective cohort study conducted in Sweden showed that water birth did not increase the number of admissions to the NICU or cause a difference in neonatal Apgar scores (Ulfsdottir et al., 2018).
Nevertheless, a comparative study between water birth and spontaneous vaginal delivery conducted in Iran showed that the mean Apgar score in the water birth group was higher than the conventional birth group with no neonatal aspirations underwater, need for prolonged hospitalization, or NICU admission. Moreover, maternal complications such as infection, postpartum hemorrhage, or readmission were not seen in women who gave birth in both groups (Akhlaghi et al., 2017). A recent meta-analysis showed that NICU admission and dystocia rates were reduced among neonates born underwater than neonates born conventionally (Zhang & Yang, 2022).
Most women lack knowledge about giving birth underwater or find it difficult to access the information about it and struggle to identify healthcare professionals willing to support their options. Therefore, healthcare providers should provide the needed information to increase the knowledge of pregnant women and their peers, explain the benefits and barriers of hydrotherapy, and follow the recommended protocols for potential candidates regarding thermoregulation of water and infection control (Dykes, 2017). In this regard, nurses and midwives have a crucial role in increasing the knowledge of pregnant women about water birth to be ready physically and mentally (Dular & Jyoti, 2019).
Previous research in Turkey showed that 39.5 % of the participants preferred water delivery. However, the percentage increased to 63.1% after watching visual media. Moreover, 70.9% of participants had insufficient information about water birth (Reyhan, 2019). In the same perspective, a study aimed to explore the perception and knowledge of women who had or did not have a water birth showed that 31% of the women who had water birth reported that their primary reasons for planning a water birth were pain relief and having a natural birth in a relaxing environment. Moreover, 69% of the women who did not have water birth reported previous obstetric complications (Lewis et al., 2018).
In summary, water birth is considered a widely available option for delivery worldwide (Milosevic et al., 2019). Unfortunately, there are few implementations of water delivery in some private hospitals in Jeddah, Saudi Arabia (Al Masoud, 2020). Further, few studies assessed water birth knowledge among medical students, staff nurses, and midwives. However, no studies evaluated public females' knowledge and perception regarding water birth in Saudi Arabia (Al Masoud, 2020; Nazir et al., 2020). Therefore, based on the limited studies and implementations, there is a knowledge and comprehension gap about water birth among women in Saudi Arabia.
Consequently, this study is pursued to shed light on the perception and knowledge level of Saudi women regarding water birth and enhance future advancements in the rate of water delivery. Furthermore, it is to determine what are the contributing factors to their knowledge level and how this can affect their decision in the future if they want a water birth. Therefore, the purpose of this research was to evaluate the perception and knowledge of Saudi women regarding water birth.
Methods
Study Design
A quantitative cross-sectional descriptive design was used in this study.
Samples/Participants
Women who matched the requirements for inclusion and completed the online data collection questionnaire were recruited for the current study. Convenience sampling was used to reach the target sample quickly. Inclusion criteria were Saudi women who are literate, more than or equal to 18 years old, married, parous, and willing to participate. While exclusion criteria were nulliparous women as they do not have previous labor experience, which may affect their knowledge and perception regarding water birth. Questionnaires completed by the nulliparous woman were not considered and got replaced. The sample size of this study was (N = 388) using the online survey system; the researchers calculated and determined the sample size using the Raosoft sample size calculator software, where input data were a number of Saudi female population was 14000000, the confidence level was 95%, and confidence interval was 5 (Raosoft, 2004).
Instruments
Data were collected using a questionnaire developed by Reyhan (2019) after granting their permission to use it. The questionnaire was forward translated from Turkish into English, then into Arabic, and was back-translated to English using competent translation services. Furthermore, it was revised accordingly by bilingual experts. The translation and back-translation ensured that the English and Arabic versions of the questionnaire were consistently asking the same questions.
The survey included four main sections. The first section included the socio-demographic features of the participants, such as age, employment status, income, and educational level. The second part elicited information on the obstetrical history as previous deliveries or abortions, as well as education about water birth. The third part assessed the perception of water birth. Lastly, the fourth part examined the knowledge of the mothers about water through a three-point ranking where each correct answer got “2”, while an incorrect answer got “0”, and an unknown answer got “1”. Incorrect items were reversely scored. Concerning the used scoring system for the level of knowledge, total scores were classified into three categories of poor for the percentage range of less than 33.3% (<33.3%), fair for 33.34-66.6%, and good for more than 66.7% (>66.7%).
The survey included four main sections. The first section included the socio-demographic features of the participants, such as age, employment status, income, and educational level. The second part elicited information on the obstetrical history as previous deliveries or abortions, as well as education about water birth. The third part assessed the perception of water birth. Lastly, the fourth part examined the knowledge of the mothers about water through a three-point ranking where each correct answer got “2", while an incorrect answer got “0”, and an unknown answer got "1". Incorrect items were reversely scored. Concerning the used scoring system for the level of knowledge, total scores were classified into three categories of poor for the percentage range of less than 33.3% (<33.3%), fair for 33.34-66.6%, and good for more than 66.7% (>66.7%).
The validity of the translated questionnaire was confirmed by a panel of content experts who were selected based on their qualifications and experience in nursing research, nursing education, and obstetrics and gynecology. They were asked to ensure the accuracy of the questionnaire, in addition to rating each item in the questionnaire in terms of its relevancy to the underlying construct and clarity on a 4-point ordinal scale. I-CVI was computed as the number of experts gave a rate of either 3 or 4 divided by the total number of experts. Afterward, S-CVI/Ave was calculated to be 0.90, which is acceptable (Lynn, 1986; Polit & Beck, 2004). There were no major amendments except reducing some items to decrease redundancy.
Moreover, a pilot study was conducted by pre-testing the validated questionnaire on 10% of the sample (39 women) who matched the requirements for inclusion to evaluate the completeness and accuracy of the survey and ensure its reliability, in addition to the clarity of its items (Polit & Beck, 2018). The reliability of the questionnaire was ensured by using a Cronbach alpha coefficient that was 0.70, reflecting its consistency.
Data Collection
The questionnaire was distributed during the period between February and March 2020 by the researchers to the Saudi women through a link supported by Google form through common social media platforms such as “Twitter app, email, and WhatsApp.” Before completing the questionnaire, the participants were able to read the inclusion criteria so they could recognize whether they could participate or not. After the participants completed the questionnaires, data were transferred automatically to the sheet application. The questionnaire was left available online until completed by 388 women who matched the requirements for inclusion in this research.
Data Analysis
The collected data were encoded and analyzed using IBM SPSS Statistics (version 23) predictive analytics software (IBM Corp., Armonk, N.Y., USA). Descriptive statistics such as frequencies, percentages, means, and standard deviations were used to present the data. Additionally, inferential statistics such as Chi-Square, Fisher Exact, and t-tests for independent samples were performed to assess the significance of comparison and association between the study's quantitative and qualitative variables. The threshold for significance was set at p <0.05.
Ethical Consideration
The study was performed after the research proposal was approved by the Research Unit-College of Nursing, King Abdullah International Medical Research Center (KAIMRC), and the Institutional Review Board (IRB) at King Abdulaziz Medical City-Western Region, Jeddah, Saudi Arabia (SP20/018/J & JED-20-427780-31661). Each woman who met the inclusion criteria and was willing to participate in the current study was informed online about the nature of the research and its aim before completing the data collection questionnaire. The informed consent was placed at the beginning of the questionnaire. Also, the participant's privacy, autonomy, and confidentiality were maintained.
Results
The mean age of the participants was 34.91 ± 8.851, with 83.2% being highly educated. Nearly half of them, 52.1%, were housewives, while 13.6% were working in health-related jobs. More than half of the participants lived in Jeddah, 58.2%, and 41.8% were from other regions. Over one-third of the participants, 35.1%, had a monthly income between 5000 – 10,000 S.R with a mean of 2.03 ± 0.807 (Table 1).
| Sociodemographic Characteristics | n | % |
|---|---|---|
|
Age (in years) Equal and below 20 21 to 30 31 to 40 Equal and above 41 Mean and standard deviation |
3 134 157 94 34.91 ± 8.851 |
0.8 34.4 40.4 24.4 |
|
Educational level Primary education Secondary education University education |
5 60 323 |
1.3 15.5 83.2 |
|
Employment status Housewife Health-related job Non-health related job |
202 53 133 |
52.1 13.6 34.3 |
|
Residence Inside Jeddah Outside Jeddah |
226 162 |
58.2 41.8 |
|
Outside Jeddah (n = 162) Makkah Asir Al jauuf Riyadh Al bahah Madinah Najran Qasim Tabuk Eastern province Jizan |
59 7 1 29 2 14 7 6 3 27 7 |
15.2 1.8 0.3 7.5 0.5 3.6 1.8 1.5 0.8 7.0 1.8 |
|
Income < 5000 S.R 5000 – 10,000 S.R > 10,000 S.R Mean and standard deviation |
121 136 131 2.03 ± 0.807 |
31.2 35.1 33.7 |
Note: age and other continuous variables were divided by grouping values into nearly equal-sized categories for descriptive purposes
| Obstetrical History | n | % |
|---|---|---|
|
The number of deliveries 0 – 4 5 – 9 10 – 15 Mean and standard deviation |
288 95 5 3.36 ± 2.167 |
74.2 24.5 1.3 |
|
The number of abortions 0 1 – 4 5 – 8 9 – 12 ≥ 13 Mean and standard deviation |
233 152 2 0 1 0.67 ± 1.159 |
60 39.1 0.6 0 0.3 |
|
Place of a previous delivery Home Hospital |
8 380 |
2.1 97.9 |
|
Prior delivery methods Spontaneous vaginal delivery (SVD) Instrumental vaginal delivery C-section |
254 34 100 |
65.5 8.7 25.8 |
|
Receiving educational courses Yes No |
166 222 |
42.8 57.2 |
|
The place of educational courses (n = 166) Special course Hospital Family health center Other |
23 46 9 88 |
13.9 27.7 5.4 53.0 |
|
Whom gave the educational courses (n = 166) Midwife – nurse Family doctor Obstetrician Other |
20 9 21 116 |
12.0 5.4 12.7 69.9 |
|
Any information about water birth was given (n = 166) Yes No |
60 106 |
36.1 63.9 |
|
Heard about water birth Yes No |
326 62 |
84 16 |
|
Source of water birth information (n = 326) Television Internet Husband, acquaintance Physician, midwife, nurse |
37 244 21 24 |
11.3 74.8 6.4 7.4 |
It was determined that the mean number of deliveries was 3.36 ± 2.167, with 60% having no history of abortion, 97.9% delivering in hospitals, 65.5% having a normal vaginal delivery, and 25.8% having a cesarean section. Furthermore, it was found that 42.8% of the participants received education on pregnancy and delivery, with 27.7% of them having their education sessions in a hospital setting and 36.1% receiving information on water birth. Furthermore, most of the participants, 84%, have heard about water birth, with 74.8% have listened on the internet (Table 2).
| Knowledge | Correct (2) (%) | Incorrect (0) (%) | Unknown (1) (%) | |
|---|---|---|---|---|
| Water birth is recommended after 37 weeks. | 56 (14.4) | 19 (4.9) | 313 (80.7) | |
| Water birth reduces birth pain. | 218 (56.2) | 7 (1.8) | 163 (42.0) | |
| Water birth increases the duration of the delivery. | 22 (5.7) | 119 (30.7) | 247 (63.6) | |
| In water birth, the increase in blood flow to the uterus increases the effect of contractions. | 73 (18.8) | 21 (5.4) | 294 (75.8) | |
| Water birth increases the rate of perineal tears. | 9 (2.3) | 119 (30.7) | 260 (67.0) | |
| Water birth reduces the use of painkillers at birth. | 132 (34) | 9 (2.3) | 247 (63.7) | |
| In water birth, the water slows cervical dilatation. | 12 (3.1) | 103 (26.5) | 273 (70.4) | |
| Cervical dilatation should be 4 cm for the mother to be taken into the birth pool. | 50 (12.9) | 10 (2.6) | 328 (84.5) | |
| In water birth, birth pains start and stay until the baby is born. | 86 (22.2) | 29 (7.5) | 273 (70.3) | |
| In water birth, the placenta and umbilical cord are delivered in the birth pool. | 80 (20.6) | 20 (5.2) | 288 (74.2) | |
| In water birth, the risk of maternal infection is the same as in normal vaginal delivery. | 43 (11.1) | 49 (12.6) | 296 (76.3) | |
| In water birth, the temperature of the water is higher than the mother's body temperature, causing a decrease in blood flow to the uterus. | 39 (10.1) | 38 (9.7) | 311 (80.2) | |
| In water birth, the water temperature is higher than the mother's body temperature, causing more maternal fluid loss. | 19 (4.9) | 53 (13.7) | 316 (81.4) | |
| Water birth increases the risk of postpartum bleeding. | 18 (4.6) | 96 (24.7) | 274 (70.7) | |
| In water birth, the mother feels she is controlling her delivery, which enhances emotional well-being. | 134 (34.5) | 7 (1.8) | 247 (63.7) | |
| Water birth allows the mother to move into various positions to relax her muscles. | 193 (49.7) | 5 (1.3) | 190 (49) | |
| Birth in water increases maternal tension. | 27 (7) | 160 (41.2) | 201 (51.8) | |
| In water birth, no medical intervention applies to the mother. | 69 (17.8) | 68 (17.5) | 251 (64.7) | |
| In water birth, the mother is passive; everything is done by the health care provider. | 19 (4.9) | 162 (41.8) | 207 (53.3) | |
| Water birth increases the mother's self-confidence | 146 (37.6) | 13 (3.4) | 229 (59) | |
| In water birth, the umbilical cord is cut 3-5 minutes after birth. | 55 (14.2) | 13 (3.4) | 320 (82.4) | |
| In water birth, the baby does not experience sudden fear and separation shock due to a late umbilical cord cut. | 94 (24.3) | 11 (2.8) | 283 (72.9) | |
| In water birth, the baby is born more easily | 180 (46.4) | 5 (1.3) | 203 (52.3) | |
| In water delivery, the possibility of newborn infection is the same as in normal vaginal birth. | 56 (14.4) | 41 (10.6) | 291 (75) | |
| In water birth, there is no possibility of neonatal aspiration or drowning. | 99 (25.5) | 60 (15.5) | 229 (59) | |
| In water birth, the passage of the fetus from a liquid medium back to a liquid medium prevents damage to the brain cells. | 51 (13.1) | 8 (2.1) | 329 (84.8) | |
| In water birth, the umbilical cord is likely to break. | 10 (2.6) | 75 (19.3) | 303 (78.1) | |
| Water birth increases the risk of trauma or injury to the mother or the newborn. | 10 (2.6) | 118 (30.4) | 260 (67) | |
| In water birth, the fetus receives much more oxygen as the maternal blood flow increases. | 58 (14.9) | 11 (2.8) | 319 (82.3) | |
| In water birth, it is more difficult to breastfeed the newborn after delivery. | 14 (3.6) | 129 (33.3) | 245 (63.1) | |
| In water birth, no additive is added to the pool water. | 70 (18) | 21 (5.5) | 297 (76.5) | |
| The presence of husbands beside women during water birth affects women positively. | 184 (47.4) | 24 (6.2) | 180 (46.4) | |
|
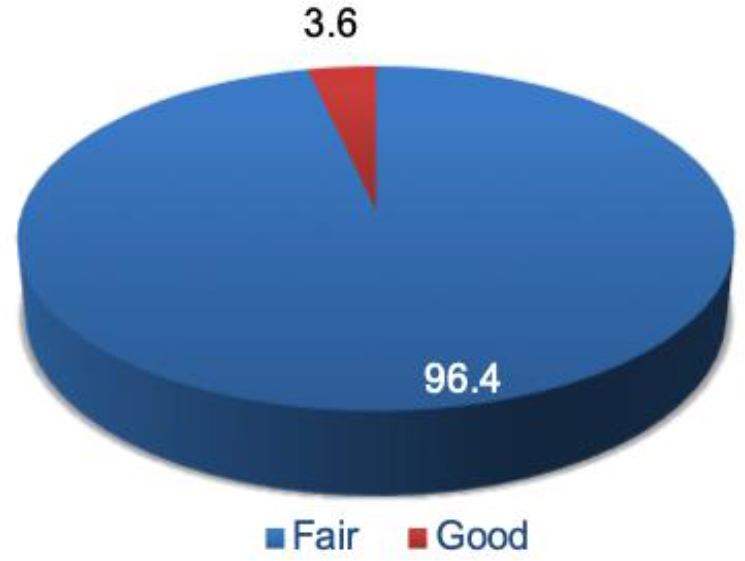
Score classification: Good: >66.7% (n = 14; 3.6%) Fair: 33.34-66.6% (n = 373; 96.4%) |
||||
Concerning knowledge of the participants on water birth, nearly half of them identified that water birth reduces birth pain and allows the mother to move into various positions for the relaxation. Also, the presence of the husband during water birth affects women positively (56.2%, 49.7% & 47.4%, respectively). On the other hand, nearly one-third of them reported that water birth increases labor duration, perineal tears, and maternal tension (30.7%, 30.7% & 41.2%, respectively) (Table 3). Figure 1 illustrates the distribution of women's knowledge of water birth based on the scoring scale; 96.4% had a fair level, and 3.6% had a good level.
| Perception regarding water birth | n | % |
|---|---|---|
|
Do you think that water birth is performed in the country? Yes No I don't know |
100 166 122 |
25.8 42.8 31.4 |
|
Do you want water birth to be a common birth method in the country? Yes No I don't know |
157 61 170 |
40.5 15.7 43.8 |
|
Do you want to give birth in water? Yes No I don't know |
156 159 73 |
40.2 41.0 18.8 |
|
Who do you want to be a companion from your family during a water birth? (n = 156) My husband My mother/sister I do not want anyone Other |
123 3 25 237 |
31.7 0.7 6.4 61.2 |
|
Who should conduct a water birth? Obstetrician Midwife / Nurse Both I do not know |
58 33 250 47 |
14.9 8.5 64.4 12.2 |
|
Do you want to have more information about water birth? Yes No |
292 96 |
75.3 24.7 |
Regarding the perception of the participants of water birth, 42.8% thought that water birth is not performed in Saudi Arabia, whereas 40.5% wanted water birth to be a common birth method in the country. Moreover, 40.2% of the women wanted to give birth in water, with 31.7% of them preferred their spouses to be their birth partners. Two-thirds of the participants, 64.4%, perceived that obstetricians and nurses should conduct water birth, and 75.3% wanted to have more information on water birth (Table 4).
| Sociodemographic characteristics | Knowledge | p-value | |
|---|---|---|---|
| % Fair | % Good | ||
| Age (mean) | 34.7 | 39.7 | 0.038* |
| Educational level | |||
| Elementary education | 80.0 | 20.0 | 0.165 |
| intermediate education | 95.0 | 5.0 | |
| College Education | 96.9 | 3.1 | |
| Recruitment status | |||
| Housewife | 95.5 | 4.5 | 0.608 |
| Health-related job | 98.1 | 1.9 | |
| Non-health related job | 97.0 | 3.0 | |
| Residence | |||
| Inside Jeddah | 96.5 | 3.5 | 0.932 |
| Outside Jeddah | 96.3 | 3.7 | |
| Salary per month | |||
| Less than 5000 SR | 95.9 | 4.1 | 0.943 |
| From 5000 to 10000 SR | 96.3 | 3.7 | |
| More than 10000 SR | 96.9 | 3.1 | |
Regarding the contributing factors to the participants’ knowledge of water birth, the age of women was found to be significantly related to their knowledge of water birth, as the mean age of women with good knowledge was 39.7 compared to 34.7 for women with fair knowledge. In contrast, other sociodemographic data of the participants had no significant relation to their knowledge level of water delivery (Table 5).
| Obstetrical history characteristics | Knowledge | p-value | |
|---|---|---|---|
| Fair | Good | ||
| Number of deliveries | 3.3 | 4.3 | 0.081 |
| Number of abortions | 0.6 | 0.8 | 0.392 |
| Place of a previous delivery | |||
| Home | 50.0 | 50.0 | 0.087 |
| Hospital | 96.6 | 3.4 | |
| Other | 100 | 0 | |
| Prior delivery methods | |||
| Spontaneous vaginal delivery (SVD) | 97.2 | 2.8 | 0.336 |
| Instrumental vaginal delivery | 97.1 | 2.9 | |
| C-section | 94.0 | 6.0 | |
| Did you receive courses about pregnancy and delivery? | |||
| Yes | 95.2 | 4.8 | 0.285 |
| No | 97.3 | 2.7 | |
| Where was the place of educational courses? | |||
| Special course | 100 | 0 | 0.009* |
| Hospital | 91.3 | 8.7 | |
| Family health center | 77.8 | 22.2 | |
| Other | 95.7 | 4.3 | |
| Who gave the educational courses? | |||
| Midwife - nurse | 95.0 | 5.0 | 0.048* |
| Family physician | 88.9 | 11.1 | |
| Obstetrician | 85.7 | 14.3 | |
| Other | 97.9 | 2.1 | |
| Any information about water birth was given to you? | |||
| Yes | 98.3 | 1.7 | 0.024* |
| No | 93.9 | 6.1 | |
| Perception of water birth | Knowledge | p-value | |
|---|---|---|---|
| Fair | Good | ||
| Do you think that water birth is performed in the country? | |||
| Yes | 98.0 | 2.0 | 0.128 |
| No | 94.0 | 6.0 | |
| I don’t know | 98.4 | 1.6 | |
| Do you want water birth to be a common birth method in the country? | |||
| Yes | 96.8 | 3.2 | 0.403 |
| No | 93.4 | 6.6 | |
| I don’t know | 97.1 | 2.9 | |
| Do you want to give birth in water? | |||
| Yes | 98.1 | 1.9 | 0.173 |
| No | 96.2 | 3.8 | |
| I don’t know | 93.2 | 6.8 | |
| Who do you want to be a companion from your family during a water birth? | |||
| My husband | 96.7 | 3.3 | 0.683 |
| My mother/sister | 92.9 | 7.1 | |
| I don't want anyone | 96.9 | 3.1 | |
| Other | 100 | 0 | |
| Who should conduct a water birth? | |||
| Obstetrician | 89.7 | 10.3 | 0.030* |
| Midwife / Nurse | 97.0 | 3.0 | |
| Both | 97.2 | 2.8 | |
| I do not know | 100 | 0 | |
| Do you want to have more information about water birth? | |||
| Yes | 96.9 | 3.1 | 0.348 |
| No | 94.8 | 5.2 | |
Furthermore, the majority of the participants who had fair knowledge received educational courses by midwives/nurses and perceived that water birth should be conducted by both the obstetrician and midwife with statistically significant relationships (95%, 97.2%; p = 0.048, 0.030 respectively) (Table 6 & Table 7).
Discussion
Considering the educational level of the participants, it was determined in the current study that the majority of the females who had a fair level of knowledge regarding water delivery had a university education with no statistically significant relationship. This may reflect that water birth is not adequately covered in the educational field, either in hospitals or schools/universities. In contrast, a study by Reyhan (2019) to identify the knowledge level regarding giving birth in the water among pregnant women showed a statistically significant correlation between women’s knowledge of water birth and a high level of education.
The location of residence was another variable that did not show any significant association with women’s knowledge. It was found that most women who lived in Jeddah had a fair knowledge of water birth, while most of the females who lived in other regions had a fair level of knowledge. This indicates that the place of residence does not affect women’s knowledge level, which may be attributed to the similarity of information resources. On the other hand, Reyhan (2019) reported a high knowledge level related to water birth among pregnant mothers whose residency is in the center of the city with a significant statistical correlation. This can be attributed to the availability of health care services and educational classes in city centers.
The age of the women in the present study was found to be significantly correlated with their knowledge about water birth. Similarly, Reyhan (2019) found a significant statistical correlation between the age of the participants and their level of knowledge of water delivery. On the other hand, no significant relationships were found between employment status, income, and women’s level of knowledge on water delivery. Similarly, Reyhan (2019) reported that the highest level of knowledge regarding water delivery was observed among employed pregnant women and those with a good family income with no statistically significant relationship.
It was found that most of the women who received educational courses on labor and delivery had a fair knowledge level about water birth with a statistically significant relationship. This finding was agreed by Reyhan (2019), who found that women with a good knowledge level about water delivery had received information and health education on water birth during their pregnancy with a statistically significant relationship.
Based on the used scoring system to determine the level of knowledge on water birth among Saudi females, it has been found that the majority of the participants had a fair level. This may reflect the importance of disseminating more information and arranging educational programs on birth modalities, including water birth. In the same regard, Reyhan (2019) reported that nearly three-quarters of the participants had insufficient information on water birth. Additionally, Carlsson and Ulfsdottir (2020) conducted a study to explore the retrospective experiences of women who had a water birth in Sweden; they reported that respondents had a lack of general and specific information related to waterbirths.
In the current research, more than half of the women reported that water birth reduces birth pain and allows the mother to move into various positions for the relaxation. Similarly, other studies revealed numerous maternal benefits of water birth as an efficient non-pharmacological modality that alleviated the sensation of pain (Brooks, 2018; Carlsson & Ulfsdottir, 2020; Cooper & Warland, 2019; Reyhan, 2019), noninvasive birth experience (Estuardo et al., 2021; Reyhan, 2019), a peaceful, calm, and relaxing method for delivery, an effective way to relieve labor discomforts (Carlsson & Ulfsdottir, 2020; Cooper & Warland, 2019) and promote labor progress (Carlsson & Ulfsdottir, 2020).
Previous studies suggested maternal complications such as infection, perineal laceration, NICU admission, and postpartum hemorrhage were less observed in women who gave birth in water (Akhlaghi et al., 2017; Sidebottom et al., 2020). Further, a retrospective study was conducted to compare water birth with a traditional delivery method in Mexico and determine both approaches’ obstetric and newborn outcomes and related complications. The authors reported no difference between the groups regarding the incidence of postpartum hemorrhage and advanced stages of perineal tears. Moreover, water birth has non-significant maternal or neonatal adverse effects (Estuardo et al., 2021). Alternatively, water aspirations, postpartum hemorrhage, advanced stages of perineal tears, maternal or newborn infection, and retained placenta were observed among water birth parturients in other studies (Brooks, 2018; Cooper & Warland, 2019; Lim et al., 2016). In the current study, it had been reported by the women that water birth does not increase the rate of perineal tears, the risk of maternal infection, and postpartum hemorrhage. Furthermore, the participants mentioned that the risk of neonatal infection is the same as normal vaginal birth, there is no possibility of neonatal aspiration or drowning, and water delivery does not raise the risk of trauma or injury to the mother or the newborn.
In the current study, less than one-third of the women thought that water birth was performed in Saudi Arabia, and more than one-third wanted water birth to be a common birth method performed for every Saudi woman. Moreover, three-quarters of the participants desired more information on water birth, and more than one-third wanted to deliver in water. Similarly, it was found that 39.5% of pregnant mothers wanted a water birth as an option for delivery (Reyhan, 2019). Another study reported that 38% of the women planned for water birth as the first choice for delivery (Lewis et al., 2018). These findings may indicate that Saudi women need to be more aware of water delivery as one of the options. Besides, nearly one-third of the participants reported that they preferred their spouses as birth companions throughout water birth. In the same line, it was reported that a considerable number of pregnant women preferred that their spouses be available throughout the moment of water birth (Reyhan, 2019). Further, the presence of the partners was described by the participants as a positive experience, and the couples became more united and intimate with the growth of genuine, humanistic, encouraging, and trustworthy relationship of care because of this presence (de Camargo et al., 2022).
Implications of the Study
Since the knowledge level among women was fair, it is recommended that educational programs on water birth need to be provided to women to help them make informed decisions about all available delivery methods, including water birth. Moreover, healthcare givers such as midwives, nurses, family physicians, and obstetricians need to broaden their knowledge about water birth, including benefits, indications, and contraindications. In addition, the private and government hospitals in Saudi Arabia offer water birth as an option for delivery to enhance the natural process and reduce intrapartum complications.
Limitations
The research faced certain limitations in collecting the data using an online survey because of COVID-19 restrictions that might impact the credibility of the answers. In addition, non-probability sampling might decrease the representativeness of the intended population and affect the generalizability of the findings. Also, there were limited studies in Saudi Arabia addressing water birth in general and the knowledge level and perception about it among females in specific.
Conclusion
Based on the findings of the current study, it can be concluded that most Saudi women had a fair knowledge level of water birth; however, they wanted to have more information on it. Furthermore, the knowledge level of women had increased with age and receiving educational courses on labor and delivery.