Background
Cervical cancer remains a global public health problem, specifically in developing countries, including Thailand. Nowadays, approximately 9,158 Thai women are annually identified as new cases of cervical cancer, and about 4,705 Thai women die from cervical cancer (International Agency for Research on Cancer, 2020). Cervical cancer, one of the few cancers, can be preventable if it is diagnosed and treated in the early stages. Cervical cytology (Papanicolaou, or Pap smear) is still widely used as a primary screening method to detect abnormalities of the cervix. For several decades, controlling cervical cancer focused on campaigns to promote women to take part in cervical cancer screening. Increased cervical screening rate leads to an increase in the prevalence of women with abnormal cervical cytology results as well. The data from the National Cancer Institute (NCI) showed the number of Thai women with abnormal cervical cytology increased from 1.13% to 1.53% during 2010-2014, according to the proportion of Thai women screened (Ploysawang et al., 2021). Presently, the prevalence of Thai women with abnormal cervical cytology results was approximately 6-7% of all women screened (Jerachotechueantaveechai et al., 2015; Tangjitgamol et al., 2016). Although the prevalence of women with abnormal cervical cytology results was not relatively high, these women were likely to be at higher risk for cervical carcinoma. If the women do not receive the continuum of care, the women may develop invasive cervical cancer in the future.
Previous studies showed that most women first receiving abnormal cervical cytology results experienced high anxiety (Ciavattini et al., 2021; O'Connor et al., 2016; Thangarajah et al., 2016). Some women were worried about their results, whereas others felt anxious about colposcopy examinations (Wittenborn et al., 2022). Most of the women with abnormal Pap smear results were worried about getting cervical cancer (Treewiriyanuphab et al., 2021). However, most Thai women with abnormal cervical cytology results could not distinguish the difference in severity levels of abnormal cervical cells, so anxiety levels were not associated with severity levels of abnormal cervical cytology results (Phuakpoolpol et al., 2018). Although the overall health-related quality of life (HRQoL) of women with abnormal Pap smear results was not reduced, a notification of an abnormal cervical cytology result and referral for colposcopy examination were correlated with anxiety and slightly impaired psychosocial aspects of HRQoL (Rask et al., 2019).
Moreover, anxiety was found to be the most common dominant emotion during the initial period (Ciavattini et al., 2021). According to Martinez-Gutierrez et al. (2023), psychological factors were associated with follow-up adherence in women with abnormal Pap tests. In other words, inadequate knowledge and adverse emotions toward colposcopy and test results were indicated as obstacles to follow-up compliance (Sansoni et al., 2022). Therefore, nurses play an important role in counseling and psychological support for those women.
From a qualitative study, women with abnormal Pap smear results required individualized oral information (Rask et al., 2017). In addition, the women directly needed health advice from nurses (Pornsinsiriruck et al., 2022). Prior studies indicated that providing educational intervention through leaflets, mail, phone, or video information did not significantly reduce anxiety in women attending colposcopy clinics (De Bie et al., 2011; Howells et al., 1999; Ketelaars et al., 2017). Consistent with the study of Wouters et al. (2019), using an animation video not only relieves anxiety or increases satisfaction in women with abnormal cervical cytology but could also reduce consultation time before colposcopy examination. It was congruent with some previous studies that showed that providing information increased knowledge but could not reduce anxiety in women with abnormal cervical cytology results (De Bie et al., 2011; Ngu et al., 2018). However, anxiety tended to decrease over time regardless of the educational interventions (Ngu et al., 2018). Likewise, women with abnormal cervical cytology results had considerable initial anxiety that reduced over time, irrespective of their management (Fielding et al., 2017).
Most studies focused on educational intervention and adherence to colposcopic follow-up among women with abnormal Pap tests. Since abnormal cervical cells were sensitive and stigmatized issues, applying one-on-one counseling in this study was appropriate for those women to reduce anxiety. Nowadays, there are few studies regarding counseling provision for women with abnormal cervical cytology results to relieve anxiety. One study examined the effect of counseling on anxiety in Thai women with abnormal cervical cancer screening by using pretest and posttest design (Chotpadiwetkul, 2020); nevertheless, there are no internationally published studies on counseling among women with abnormal cervical cytology results.
Establishing rapport between a woman and a nurse is essential to providing effective counseling for those women. The feminist model was used to guide the counseling for women with abnormal Pap smears because nurses are also women congruent with the sub-concepts of this model, which included 1) symmetry in provider-patient relationships, 2) access to information, 3) shared decision-making, and 4) social change. In addition, a feminist model for women’s health care (Andrist, 1997) had never been used in the group of women with abnormal cervical cytology; as a result, this model was integrated into this study to achieve comprehensive health care. Thus, the purpose of this study was to investigate the effect of colposcopy counseling with a feminist model on anxiety in Thai women with abnormal cervical cytology results.
Methods
Study Design
A time-series quasi-experimental design with a comparison group guided by the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) checklist (Des Jarlais et al., 2004) was applied in this study. The study was conducted at the colposcopy clinic of a university hospital in Bangkok, Thailand, from August 2022 to April 2023.
Samples/Participants
The participants were purposively selected following the inclusion criteria by using purposive sampling. The eligible participants of this study were 1) Thai women with abnormal cervical cytology results, 2) aged 18-59 years who first attended the colposcopy clinic, 3) were able to communicate and understand in Thai, and 4) were willing to participate in this study. The exclusion criteria were women who have ever had other serious gynecological problems or have a history of cervical malignancy and were currently pregnant. The sample size was calculated by using G*Power 3 (Faul et al., 2007) based on Cohen’s formula (Cohen, 1988) at a significant level of 0.05, a desired power of 0.90, and the estimated effect size of 0.80 derived from a previous study (Chotpadiwetkul, 2020). The total sample size was 56 participants. For the 12-week follow-up, 20% of the attrition rate was added to the sample size; the total sample size was about 68 participants. The total sample size was equally divided into two groups; as a result, the sample size in each group was 34 participants.
Instruments
The instruments of this study comprised two sets, namely instruments for the intervention and instruments for data collection.
First, the interventional instrument was a guide to colposcopy counseling for women with abnormal cervical cytology results. It consisted of principles of counseling, essential information, common concerns, and frequently asked questions relevant to cervical cancer and human papillomavirus (HPV), as well as dealing with potentially stigmatizing information and prevention of stigma arising in the provision of information about HPV and cervical cancer. In addition, the contents contained reporting the results of Pap tests by the 2014 Bethesda system, counseling for the women who have suspected and non-suspected cancer, diagnostic methods and treatment options for preinvasive cervical cancer, and counseling process for before, during, and after women undergoing colposcopic examination, diagnostic procedures, or treatment. A guide to colposcopy counseling was verified by five experts: two physicians who specialized in gynecologic oncology, one nursing instructor who specialized in obstetrics and gynecology care, and two registered nurses who specialized in caring for patients with gynecologic oncology problems. The Content Validity Index (CVI) for this instrument was 1.00.
Second, the instruments for data collection contained the personal information questionnaire and the State-Trait Anxiety Inventory (STAI) questionnaire as follows.
The personal information questionnaire was developed by the researcher based on the relevant literature. Demographic characteristics were age, marital status, education, occupation, financial status, health insurance, pregnancy history, the number of children, contraceptive use, history of alcohol drinking and smoking, and history of having a direct relative with cervical cancer.
The State-Trait Anxiety Inventory (STAI) questionnaire was developed by Charles D. Spielberger (Spielberger, 1983). The State-Trait Anxiety Inventory for AdultsTM (STAI-AD) was the definitive instrument for measuring anxiety in adults published by Mind Garden, Inc. The Thai version of this questionnaire had already been asked for permission to be used in this study. The self-evaluation questionnaire had 40 questions containing 20 questions of STAI Form Y-1 and 20 of STAI Form Y-2. The STAI Form Y-1 represented state anxiety, and the STAI Form Y-2 represented trait anxiety. Each question had a four-rating scale for the STAI Form Y-1 and the STAI Form Y-2. The score of each item was weighted on a 1-4 scale. The total scores of each form ranged from 20 - 80. The higher scores indicated a higher level of anxiety. The reliability of STAI Form Y-1 and STAI Form Y-2 tested with 30 Thai women with abnormal cervical cytology results was excellent, with Cronbach’s alpha coefficient of 0.93 and 0.90, respectively.
Interventions
The manual of colposcopy counseling was developed by the researcher as a guideline for three intervenors at a colposcopy clinic. It included the principal investigator and two nursing instructors to conduct counseling for women with abnormal cervical cytology results by applying a feminist model for women’s health care (Andrist, 1997). The standpoint of a feminist model for women’s health care contains four main themes: symmetry in provider-patient relationships, access to information, shared decision-making, and social change (Andrist, 1997).
First, the relationship between intervenors and a woman was non-hierarchical or reciprocal as partners by minimizing traditional physical, social, and personal barriers and attentively listening to women’s stories. Second, access to information was the way in which the information was delivered and facilitated by the intervenors and available other resources. Prior to sharing the information, the intervenors assessed patients’ knowledge, self-care behaviors, and thoughts, as well as be able to detect when their message was not obvious. So, the intervenors needed to listen to women’s life-world. Third, when the women became knowledgeable participants, they could participate in healthcare decision-making. Also, building mutual trust was a key element of the feminist model in shared decision-making. Last, the intervenors treated women as patient-centered; when they trusted the system, they were strong in practice pertaining to women’s health care (Andrist, 1997). The experimental group received one counseling session at the first attendance because the women had high anxiety during the initial period after perceiving their results. The counseling was conducted in a private and quiet room at the colposcopy clinic and took 45-60 minutes.
In contrast, the comparison group was referred to routine care that women with abnormal cervical cytology results received during their visit to the colposcopy clinic. The service they received from the routine care was health education via video and brochure about care in colposcopy on the first day they visited the clinic.
Data Collection
After receiving IRB approval, participants who gained detailed research information and were willing to participate in this study were asked to sign the written consent form. The researcher trained two registered nurses who were research assistants to collect the baseline data in both groups. However, two registered nurses collecting the data did not conduct the counseling session.
The researcher assistants recruited and invited the eligible participants according to the inclusion criteria. After the eligible participants gained the information related to the study and were willing to participate, the researcher assistants divided the participants into two groups: the participants willing to receive counseling were the experimental group, and the others not preferring to receive counseling were the comparison group.
The study was conducted simultaneously in both groups. The data were compiled using self-administered questionnaires, including personal information and anxiety (STAI FORM Y-1 and FORM Y-2) at baseline before providing the usual care for both groups. Both groups received the usual care. For the comparison group, participants obtained only the usual care. For the experimental group, the researcher provided colposcopy counseling plus the usual care for the participants in the research setting.
Furthermore, the researcher and two nursing instructors conducted a consultation according to a guide to colposcopy counseling with a feminist model. As for the posttest data, state anxiety (STAI FORM Y-1) was assessed immediately after completing the usual care and colposcopy counseling by the research assistants in both groups. In the 12th week after the intervention implementation, state anxiety was assessed by the researcher assistants in both groups via telephone calls. The flow diagram of the study between the experimental group and the comparison group among Thai women with abnormal cervical cytology results was summarized as illustrated in Figure 1.
Data Analysis
The IBM SPSS Statistics for Windows (Version 21.0) was applied to analyze the data. Data were analyzed using descriptive statistics, the Chi-square test, and the independent t-test to compare the difference between the experimental and comparison groups on demographic characteristics, state and trait anxiety at baseline assessment. The assumptions for those statistics were met before analyzing the t-test and the repeated measures ANOVA. To determine the effect of colposcopy counseling, state anxiety as a dependent variable was analyzed by using one-way and two-way repeated measures ANOVA to test the difference of mean scores at different time points.
Ethical Consideration
The research proposal was approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Thailand, with the approval number COA. MURA2022/394. Participants were informed regarding the purposes of the study, the information relevant to the study, and the pros and cons they gained to weigh the risks and benefits. Their participation was voluntary, and they were asked to sign the written consent form. During the study, participants could decline their participation until data collection was concluded. All participants’ data were kept confidential by the researcher in a locked cabinet. Their names were not displayed on the questionnaires, and the number coding was used instead of the names of participants. The results of this study were presented only in the whole overview and based on academic purposes.
Results
The participants in both groups ranged from 23 to 57 years old, with an average age of 36.15 (SD = 9.00) in the comparison group and 39.97 (SD = 10.14) in the experimental group. More than half of the participants in the comparison group were single, separated, and divorced, while half of the participants in the experimental group were married. Most participants in both groups had a bachelor’s degree and higher, were employees, and had sufficient money. Most of the participant’s health insurance in both groups were universal coverage schemes and social security schemes. Most of the participants in the comparison group had never been pregnant (52.94%), whereas most of the participants in the experimental group had ever been pregnant but had never been abortive (41.18%). Likewise, most of the participants in the comparison group did not have children (58.82%), but most participants in the experimental group had children (58.82%). The majority of the participants in both groups used to take birth control. At present, most participants in both groups did not take birth control. Most participants in both groups did not drink alcohol or smoke as well as had never had a direct relative with cervical cancer. The results showed that there were no statistical differences in demographic characteristics between the two groups (p >0.05), as presented in Table 1.
| Demographic characteristics | Comparison group | Experimental group | Statistics value | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age (years) | Mean = 36.15, SD = 9.00, min-max = 24 – 54 | Mean = 39.97, SD = 10.14, min-max = 23 – 57 | -1.644c | 0.105 | ||
| Marital status | 0.237a | 0.626 | ||||
| Single/separated/ divorced | 20 | 58.80 | 17 | 50.00 | ||
| Married | 14 | 41.20 | 17 | 50.00 | ||
| Education | 0.082a | 0.775 | ||||
| Less than bachelor’s degree | 7 | 20.60 | 9 | 26.50 | ||
| Bachelor’s degree and higher | 27 | 79.40 | 25 | 73.50 | ||
| Occupation | 2.857a | 0.240 | ||||
| Unemployed | 5 | 14.70 | 10 | 29.40 | ||
| Employee | 16 | 47.10 | 16 | 47.10 | ||
| Government officer | 13 | 38.20 | 8 | 23.50 | ||
| Financial status | 0.062a | 0.803 | ||||
| sufficient | 20 | 58.80 | 22 | 64.70 | ||
| insufficient | 14 | 41.20 | 12 | 35.30 | ||
| Health insurance | 0.277a | 0.871 | ||||
| Government officer and state enterprise officer | 14 | 41.20 | 12 | 35.30 | ||
| Universal coverage scheme and social security scheme | 15 | 44.10 | 16 | 47.10 | ||
| Private health insurance and self-payment | 5 | 14.70 | 6 | 17.60 | ||
| Pregnancy history | 2.152a | 0.341 | ||||
| Never be pregnant | 18 | 52.94 | 12 | 35.29 | ||
| Ever be pregnant, but never be abortive | 10 | 29.41 | 14 | 41.18 | ||
| Ever be abortive | 6 | 17.65 | 8 | 23.53 | ||
| History of having children | 1.471a | 0.225 | ||||
| No children | 20 | 58.82 | 14 | 41.18 | ||
| Having children | 14 | 41.18 | 20 | 58.82 | ||
| Contraception history | 0.434a | 0.510 | ||||
| Never taken birth control | 7 | 20.60 | 4 | 11.80 | ||
| Used to take birth control | 27 | 79.40 | 30 | 88.20 | ||
| Current methods of contraception | 3.002a | 0.223 | ||||
| No contraception | 14 | 41.20 | 21 | 61.80 | ||
| Hormonal contraception | 12 | 35.30 | 7 | 20.60 | ||
| Non-hormonal contraception | 8 | 23.50 | 6 | 17.60 | ||
| History of alcohol drinking | 0.000a | 1.000 | ||||
| No drinking | 22 | 64.70 | 22 | 64.70 | ||
| Drinking | 12 | 35.30 | 12 | 35.30 | ||
| Smoking history | - | 1.000b | ||||
| No smoking | 33 | 97.10 | 32 | 94.10 | ||
| Used to smoke | 1 | 2.90 | 2 | 5.90 | ||
| History of having a direct relative with cervical cancer | - | 0.614b | ||||
| No having | 33 | 97.10 | 31 | 91.20 | ||
| Having | 1 | 2.90 | 3 | 8.80 | ||
Comparison of Anxiety between the Comparison and Experimental Groups at Different Time Points
Before comparing state anxiety after the intervention, the researcher compared trait and state anxiety to ensure that the study results originated from the intervention. Table 2 shows no statistical differences in trait and state anxiety between the two groups at baseline (p = 0.404 and 0.157, respectively). Similarly, the results demonstrated no statistical differences in state anxiety between the two groups at the immediate and 12th week post-tests (p = 0.379 and 0.309, respectively).
| Time | Comparison group (n = 34) | Experimental group (n = 34) | t | p-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Baseline (pre-test) | ||||||
| Trait anxiety | 41.44 | 6.18 | 42.91 | 8.13 | -0.840 | 0.404 |
| State anxiety | 42.59 | 8.02 | 45.82 | 10.47 | -1.430 | 0.157 |
| Immediate post-test | ||||||
| State anxiety | 41.24 | 12.00 | 38.88 | 9.82 | 0.885 | 0.379 |
| 12th week post-test | ||||||
| State anxiety | 36.53 | 8.71 | 34.18 | 10.15 | 1.026 | 0.309 |
The Effect of Colposcopy Counseling on Anxiety
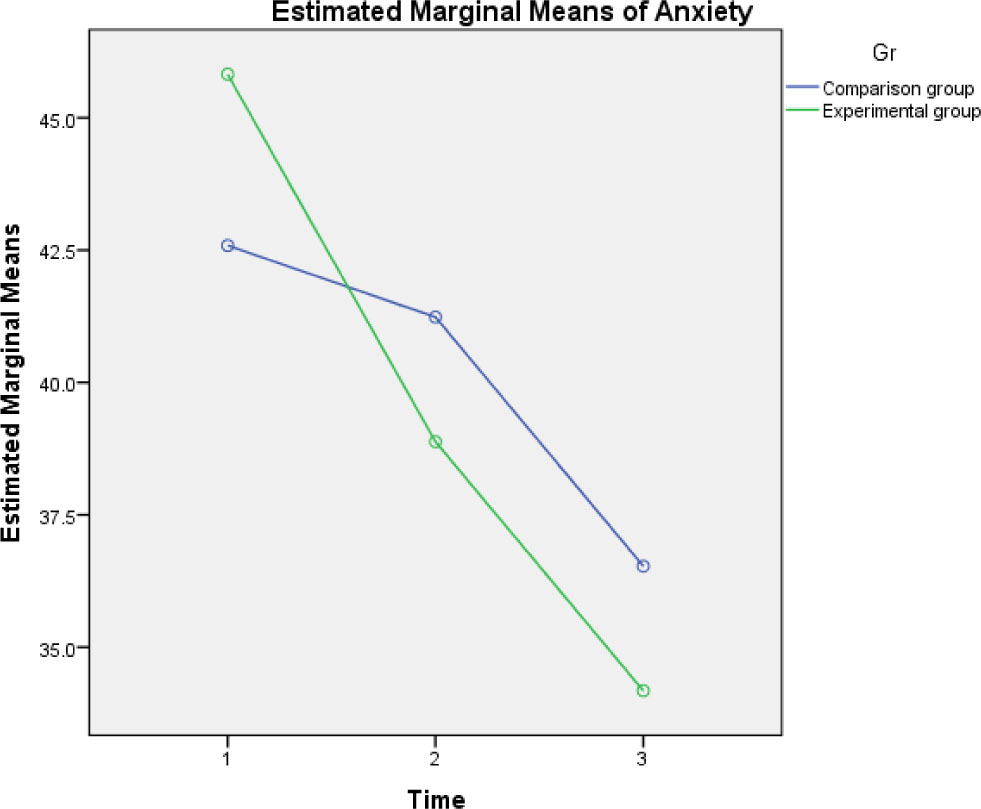
The assumptions of a repeated measures ANOVA were met before data analysis. The results indicated no significant differences in the mean anxiety score over time between the two groups (F1, 66 = 0.062, p = 0.804). However, each group showed similar results that there were significant effects of time for at least one pair across time points on the mean anxiety score (p <0.05) (Table 3). Additionally, the mean anxiety score in both groups was significantly reduced from baseline to the 12th week post-test (Figure 2).
| Time | Comparison group (n = 34) | Experimental group (n = 34) | F-test between group | p-value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | F-test within group | Mean ± SD | F-test within group | |||
| Baseline (pre-test) | 42.59 ± 8.02 | 8.374* | 45.82 ± 10.47 | 19.953* | 0.062 | 0.804 |
| Immediate post-test | 41.24 ± 12.00 | 38.88 ± 9.82 | ||||
| 12th week post-test | 36.53 ± 8.71 | 34.18 ± 10.15 | ||||
Note: *p <0.05
A comparison of anxiety of the comparison group across three points of time is displayed in Table 4. The results showed no statistical differences in state anxiety at baseline and immediate post-test (p = 0.480). Nevertheless, the mean score of anxiety at baseline was significantly higher than that at the 12th week post-test. Moreover, the mean score of anxiety at the immediate post-test was significantly higher than that at the 12th week post-test.
| Time to measure | Mean | Baseline (pre-test) | Immediate post-test | 12th week post-test |
|---|---|---|---|---|
| Baseline (pre-test) | 42.59 | |||
| Immediate post-test | 41.24 | 1.35 | ||
| 12th week post-test | 36.53 | 6.06* | 4.71* |
Note: *p <0.05
Table 5 displays the comparison of anxiety in the experimental group across three points of time, indicating that the mean score of anxiety at baseline was higher than those at the immediate post-test and 12th week post-test, respectively. In other words, anxiety was significantly decreased over time compared between baseline, immediate post-test, and 12th week post-test (p <0.05).
Discussion
Summary of the Findings
The present study indicated no significant differences in state anxiety between the comparison and experimental groups across three time points (p = 0.804). This result was congruent with the prior study in that there was no significant difference in the mean score of anxiety between the two groups after providing a decision aid (Baharvand et al., 2023). According to Baharvand et al. (2023), women’s anxiety and fear of cervical cancer, as well as low health literacy, might raise new concerns about treatment options. From the systematic review of interventions for reducing anxiety in women undergoing colposcopy, the results showed that pre-colposcopy counseling was not associated with anxiety reduction (Galaal et al., 2007). Such findings may be due to using a pre-colposcopy group session in counseling; consequently, the anxiety of individualized women was not addressed. However, one study using pre and post-test design with control revealed that participants receiving counseling had significantly lower mean scores of anxiety than those not receiving counseling (Chotpadiwetkul, 2020).
The majority of participants in this study graduated with a bachelor’s degree and higher, which might affect their understanding of the information; as a result, participants receiving counseling could reduce anxiety levels better than those not receiving counseling because participants in the experimental group gained the information that met their needs. The result of the current study might be argued that participants could access knowledge at all times through various channels, particularly the Internet, which can also alleviate participants’ anxiety. Besides, more than half of the participants in this study were well educated in that they completed a bachelor’s degree and higher, which influenced their understanding of the information. As a result, the anxiety levels were not significantly different between the two groups. On the contrary, some women might be overwhelmed with a lot of information from other sources, such as the Internet, that is easy to access, which might cause women’s concerns (Ngu et al., 2018; Rask et al., 2019). In addition, the mean ages of the participants between the two groups were similar, and they had good jobs, such as employees and government officers. This group is competent in finding information about the disease and its management. These characteristics of the participants lead to reasons that they can reduce their anxiety over time after getting the information (Ngu et al., 2018). Nevertheless, after the intervention with counseling and the comparison group receiving health education, these women were examined per vagina by physicians using colposcopy. During this time, these women were told about the diagnosis and prognosis of the abnormal cervical area, including how to be treated and continuity of follow-up. This would help to reduce the women’s anxiety over time.
Although there were no significant differences in state anxiety across three times between the two groups, anxiety in both groups was significantly decreased over time. Anxiety of women with abnormal cervical cytology reduced over time, irrespective of their management options (Fielding et al., 2017). Similarly, there was no significant difference in the psychosocial well-being of women with a positive high-risk human papillomavirus between the two groups at three-time points regardless of the intervention (i.e., leaflet provision and counseling) (Ngu et al., 2018). From the comparison of anxiety in each group across three points of time in the present study, there was at least one pair of anxiety differences. Within the comparison group, there was one pair indicating no anxiety differences in that anxiety at baseline was not significantly different from anxiety at immediate post-test.
Meanwhile, the mean score of anxiety in the experimental group significantly declined over time. According to Andrist (1997), a feminist model for women’s health care helped healthcare providers establish symmetrical relationships with women to diminish the hierarchical and patriarchal medical models. During colposcopy counseling, the healthcare providers listened attentively to women’s stories to assess their knowledge, self-care activities, and thoughts and then provided some information that met their needs. After women obtained the precise required information, healthcare providers helped increase women’s confidence in their ability to make decisions in their health care. Therefore, providing colposcopy counseling during the initial period was productive in minimizing anxiety as well as empowering women to take charge of their own health care.
Implications for Nursing Care Practice
The results can be used as evidence-based practice for professional nurses to provide comprehensive health care for women with abnormal cervical cytology results. The researcher provided the manual of colposcopy counseling as a guideline for healthcare providers to counsel women. Even though women’s anxiety naturally decreased over time, the findings indicated that colposcopy counseling applying a feminist model was useful for the women to reduce anxiety, especially during the initial period after they knew the result. Due to the high anxiety of women first perceiving abnormal cervical cytology results, nurses and other healthcare providers play a vital role in counseling and giving psychological support to the women.
Limitations of the Study
Some threats to internal validity existed within the quasi-experimental design. Lacking random assignment resulted in the selection threat and the selection-maturation interaction. Regarding threats to external validity, colposcopy counseling might be effective only in the study sample because the sample was not representative of the population. In other words, the research results generalized back to the population were limited because this study had no random selection.
Conclusion
This study found no significant differences in state anxiety between the two groups across the three-time points. However, anxiety in both groups significantly decreased over time, regardless of the intervention. Analyzing the results within the comparison group revealed that anxiety at baseline was not significantly different from that at the immediate post-test. Conversely, within the experimental group, anxiety significantly reduced over time from baseline to the 12th week post-test. Therefore, colposcopy counseling appears to be beneficial for women with abnormal cervical cytology results in reducing anxiety, particularly in the initial period. It is evident that counseling should be complemented with health education when women first visit the colposcopy clinic to decrease their anxiety promptly. Additionally, integrating a feminist model for women’s health care is recommended for all women with other diseases. For future research, considering the inclusion of women's spouses or families and the implementation of a randomized controlled trial should be taken into account.