Background
Oral feeding readiness, defined as the initial phase of oral feeding or the moment when an infant is prepared to commence oral feeding, plays a crucial role in the complex process of caring for preterm infants in the intensive care unit (Cardin et al., 2023). During this period, the transition from enteral to oral feeding takes place to meet the nutritional requirements of preterm infants (Gentle et al., 2022; Ostadi et al., 2021). The success of achieving oral feeding readiness is influenced by two sets of factors: internal factors, including neurological, gastrointestinal, cardio-respiratory, and musculoskeletal development, and external factors, including the therapeutic care environment, caregiver competence, and the infant’s stress level (Camur & Cetinkaya, 2021; Fucile & Dow, 2023).
Organ immaturity in preterm infants may result in suboptimal physiological functions. For example, the immaturity of primitive reflexes affects the risk of vomiting, irregular sucking-swallowing-breathing rhythm, airway instability during feeding, and the risk of aspiration (Costa et al., 2022). Gastrointestinal immaturity leads to preterm infants experiencing feeding intolerance, such as an increase in gastric residue of more than 50% during feeding intervals, hemorrhagic residue, abdominal distension, and discoloration around the abdomen. These factors result in increased mortality and morbidity among preterm infants, such as necrotizing enterocolitis (NEC) (Williams et al., 2023).
Oral feeding difficulties also have long-term impacts on the care process for preterm infants, including inadequate nutritional status, prolonged hospitalization, increased care costs, and disruption of mother-infant bonding attachment (Debata et al., 2022; Wahyuni et al., 2022). Impaired postnatal growth and development are also indicated as a consequence of the interaction between energy requirements, nutrients, and gastrointestinal tract immaturity (Malak et al., 2022). Furthermore, there are neurodevelopmental delays as the preterm infant matures (Buys & Gerber, 2021; Cardin et al., 2023). Nurses play a crucial role in minimizing the long-term impact of feeding difficulties during this transitional period.
Nursing interventions have been developed to enhance preterm oral feeding readiness, such as nonnutritive sucking (NNS) using pacifiers. Research results indicate that pacifier feeding can improve preterm oral feeding skills (Heller Murray et al., 2021; Li et al., 2022; Ostadi et al., 2021). However, there are still variations in research findings, with Almahrul et al. (2021) suggesting that pacifier feeding may disrupt breastfeeding or lead to oral aversion. Other nursing interventions developed include cue-based feeding, positioning, and oral-motor stimulation. The implementation of these nursing interventions has not been fully optimized in special care units (Girgin & Gözen, 2020). This is highlighted by the low level of knowledge among nurses, scoring 64.7 (out of a maximum of 100), related to the implementation of cue-based feeding interventions, oral-motor stimulation, NNS, and positioning (Girgin & Gözen, 2020). The study recommends a more in-depth exploration of the role of nurses in improving preterm oral feeding readiness.
Nurses are a crucial factor in successfully improving preterm oral feeding readiness, as they provide effective and efficient nursing care to enhance the oral feeding transition ability of preterm infants (Beissel et al., 2022). Girgin et al. (2021) emphasize the need for information to evaluate preterm oral feeding readiness, which can serve as a basis for formulating innovative nursing interventions. Nurses are responsible for providing safe interventions, minimizing negative impacts, and improving care outcomes related to preterm oral feeding readiness (Galal et al., 2023; Maastrup et al., 2021).
Several qualitative studies have been conducted to explore preterm oral feeding readiness. Descriptive research by Cardin et al. (2023) investigated the understanding of the complexities of oral feeding within a cultural context. Other qualitative studies have explored mothers’ experiences, expectations, and psychosocial needs regarding feeding (Clapton-Caputo et al., 2021; Thomson et al., 2023; Yang et al., 2022; Yu et al., 2023). Pramono et al. (2022) investigated Indonesian nurses’ experiences with successful breastfeeding, but it was not specific to preterm infants in the enteral to oral feeding transition period in special care units. Another research study, a phenomenological exploration through in-depth interviews, examined mothers’ experiences fulfilling parental roles, including feeding, in special care units (Hariati et al., 2023).
Most qualitative research conducted thus far has explored the experience of oral feeding readiness from the perspective of parents of preterm infants (Cardin et al., 2023; Clapton-Caputo et al., 2021; Hariati et al., 2023; Thomson et al., 2023; Yang et al., 2022; Yu et al., 2023). In contrast to previous studies involving parents of preterm infants admitted to special care units, the current research focuses on nurses working in special care units at levels II and III. Our study is based on the nurses’ perspectives on providing nursing care, specifically during the enteral to oral feeding transition period, to explore their experiences improving preterm oral feeding readiness in special care units.
Methods
Study Design
A qualitative descriptive study design (Doyle et al., 2020; Kim et al., 2017) was employed to explore the phenomena of nurses in more depth regarding their behavior, feelings, and experiences to answer what, how, and why the phenomena of increasing preterm oral feeding readiness admitted to the intensive care unit occurred. The research report adhered to the guidelines provided by the consolidated criteria for reporting qualitative research (COREQ) (Tong et al., 2007).
Samples/Participants
The study was conducted in a specialized referral hospital for high-risk infants in Central Java, Indonesia, which has implemented developmental care and the Family Centered Care (FCC) approach in the care of preterm infants. The hospital’s treatment room was divided into the High Care Unit (HCU) for level II preterm infants and the Neonatal Intensive Care Unit (NICU) for level III preterm infants. The research participants included nurses in the neonatal special intensive care unit. The sampling technique used was purposive sampling, aimed at gaining access to observations and conducting interviews with nurses to obtain rich data for interpretation (Holloway & Galvin, 2017). This approach also aimed to capture variations in demographic data among nurses based on their education level and the level of the neonatal special intensive care room (Haenssgen, 2019). Participant selection was criterion-based, and the inclusion criteria for the study consisted of nurses who met the following conditions: 1) possessed a minimum education level of an associate degree in nursing; 2) had at least two years of work experience; and 3) had completed training in neonatal-specific intensive care rooms for a minimum of 3 months.
Data Collection
Data were collected from January to March 2023. A semi-structured, in-depth interview method was chosen, and it was conducted by the first researcher, a pediatric nurse with experience caring for preterm infants in the special care unit. The first researcher also received training in preterm infant care management and developmental care. The purpose of using the semi-structured in-depth interview method was to explore the nurses’ perspective, including their inner thoughts and perspectives on who, where, and what factors are involved in improving preterm oral feeding readiness. These interviews were conducted face-to-face in the HCU and NICU nursing rooms. There were no other participants present in the interview room to allow for the capture of both verbal and nonverbal responses during the interview (Doyle et al., 2020).
Prior to commencing data collection, the researchers conducted a pilot interview to develop questions that aligned with the research objectives and to refine their communication skills. The results of the pilot interviews were then discussed with the supervisors (researchers 2, 3, and 4) to create interview guidelines and establish effective communication methods for conducting in-depth interviews. The interview guideline contained initial questions to facilitate the development of further questions during the interview process. The questions included: 1) What do you think about preterm oral feeding readiness? 2) What is the nurse’s experience in improving preterm oral feeding readiness? 3) What is the nursing care process to improve preterm oral feeding readiness? 4) Are there other opinions that you would like to convey in increasing preterm oral feeding readiness?
Data collection used a voice recorder, an Android smartphone for recording interviews, writing instruments, a laptop, and field note sheets. Stationery and field notes were used to document participants’ responses to questions, nonverbal communication, and keywords and terms used by the participants. Interview meetings with participants were conducted twice in the hospital discussion room. The first meeting aimed to establish a trusting relationship, provide informed consent, and agree upon the interview schedule. The second meeting involved the actual interviews. The interview typically lasted 30 to 60 minutes, and no repeat interviews were conducted. The researcher recorded verbal and nonverbal responses during the interview process in field notes. The saturation of research data was discussed with the research team (researchers 2, 3, and 4), and data were deemed saturated in the tenth participant when no new codes emerged (a total of 122 codes generated).
Data Analysis
Thematic analysis, as outlined by Kiger and Varpio (2020), was employed to analyze relevant themes to address research questions related to improving preterm oral feeding readiness through nursing care. This analysis facilitated a comprehensive exploration of nurses’ experiences, behaviors, and perspectives concerning preterm oral feeding readiness. The steps involved in thematic analysis consisted of 1) Recognizing data by reading the entire interview transcript, making notes or memos, and identifying keywords; 2) Initial coding of data, which the data were coded briefly to provide meaningful descriptions; 3) Identifying subthemes and themes by examining the list of codes and their relationships to organize codes into broader subthemes and themes, describing their significant meanings, 4) Reviewing themes, 5) Defining and naming themes, and 6) Writing the results.
Additionally, the researcher utilized the framework proposed by Abfalter et al. (2021) for the translation process, which consists of seven steps: 1) Why: The translation aimed to establish scientific value and academic interest in society for publication in international journals, 2) When: Translation occurs during the final stages of data analysis and dissemination of findings, 3) What: Research results, including meaningful statements, coding, subthemes, themes, and publication manuscripts were translated. Transcripts were not translated due to the extensive amount of text; 4) Who: The first researcher prepared the draft for translation from Indonesian to English, and an experienced external translator carried out the translation; 5) How: The translation followed a technical or forward translation approach from Indonesian to English. The first researcher, who conducted the interview data collection, prepared the results of data analysis and publication manuscripts for translation by external translators. The translated results were then validated by the second, third, and fourth researchers through comparison with the Indonesian version; 6) Where: The translation took place in the socio-geographical environment of the language source where the research data were collected to preserve the original meaning and contextual information based on the subcultural and social identities of the research participants, 7) By What Means: External translators with experience in translating qualitative health research results were employed for the translation process. Bilingual dictionaries and not IT applications were used as auxiliary tools.
Trustworthiness
The trustworthiness in this study included objectivity, dependability, credibility, transferability, and applicability (Hays & McKibben, 2021). Objectivity implies that the research was carried out in an unbiased and rational manner, involving peer debriefing and discussions with supervisors who were experts in neonatology, nursing, and nutrition. Dependability or reliability, which assesses data consistency over time, was ensured through the inquiry audit method. This method involved the participation of a supervisor in developing keywords, coding, subthemes, and themes. Credibility was maintained by verifying the truth value of the data through member checking. Feedback on the final themes was provided to all participants through email or other designated contacts. Additionally, data triangulation was performed by examining nursing records, including assessments, nursing diagnoses, planning, implementation, and evaluations. Transferability, which assesses the ability to generalize research results to the broader population, was facilitated by presenting research findings to allow readers to draw conclusions about the identified themes. Applicability involves ensuring that the research results are valid and transferable. This was achieved by preparing manuscripts that provide comprehensive information about the research findings to benefit readers.
Ethical Considerations
This research underwent ethical scrutiny and received approval from the ethical review board of Universitas Indonesia, with approval number KET-285/UN2.F12.D1.2.1/PPM.00.02/2022 on 28 December 2022. This study adhered to ethical principles by demonstrating respect for participants and allowing them the autonomy and self-determination to refuse or participate in the study. Informed consent was obtained from participants after the researcher thoroughly explained the study’s purpose, potential benefits, and procedures. Additionally, the researcher emphasized the importance of confidentiality and anonymity, safeguarding participants’ identities and data, including notes, recordings, and interview transcripts. The researchers also upheld the principle of beneficence by explaining how the research could advance scientific knowledge and took measures to minimize any potential risks, such as discomfort, during the interview process, thereby ensuring non-maleficence. The selection of participants was based on predetermined inclusion and exclusion criteria, promoting justice in the research process. Furthermore, the ethical principle of preventing exploitation was applied, ensuring that actions or activities did not unduly take advantage of participants (Holloway & Galvin, 2017).
Results
A total of ten nurses actively participated in this study, and there were no dropouts. These participants were distributed across three different rooms: four participants in the level III Neonatal Intensive Care Unit (NICU), five participants in the level II High Care Unit (HCU Neonatology), and one participant in the Comprehensive Obstetric and Neonatal Emergency Services (PONEK) room. Regarding educational background, three participants held an Associate Degree in Nursing, six had completed a Bachelor of Science in Nursing Education, and one held a Master’s Degree in Nursing. When categorizing participants based on their competency levels, following the criteria of nursing career path: novice, advanced beginner, competent, and proficient (Gunawan & Juanamasta, 2022; Ministry of Health, 2017), eight participants were classified as level III nurse practitioners (competent), while two participants were categorized as level II nurse practitioners (advanced beginners). Further details regarding participant characteristics are provided in Table 1.
| Code | Length of Work (Years) | Recent Education | Competency Qualification | Clinical Training/Experience | Unit |
|---|---|---|---|---|---|
| P1 | 19 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Neonatal Resuscitation Training, LBW Management | HCU-Neo (Level II) |
| P2 | 10 | Associate Degree in Nursing | Nurse Practitioner-II (Advanced Beginner) | Neonatal Resuscitation Training, Breastfeeding Counseling Training, Neonatal Surgical Care | HCU-Neo (Level II) |
| P3 | 19 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Neonatal Resuscitation Training, LBW Management in NICU | NICU (Level III) |
| P4 | 20 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Neonatal Resuscitation Training, LBW Management in NICU, Developmental Care Training | NICU (Level III) |
| P5 | 19 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Neonatal Resuscitation Training, Intensive Care Training | NICU (Level III) |
| P6 | 17 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Neonatal Resuscitation Training, LBW Management in NICU | NICU (Level III) |
| P7 | 17 | Associate Degree in Nursing | Nurse Practitioner-III (Competent) | Neonatal Obstetrics Emergency Life Support (NOELS) training, infant nutrition training | HCU-Neo (Level II) |
| P8 | 19 | Bachelor of Science in Nursing | Nurse Practitioner-III (Competent) | Kangaroo Care and LBW Management Training | HCU-Neo (Level II) |
| P9 | 11 | Associate Degree in Nursing | Nurse Practitioner-II (Advanced Beginner) | Neonatal Resuscitation Training, CPAP Attached Preterm Infant Management Training | HCU-Neo (Level II) |
| P10 | 12 | Master’s Degree in Nursing | Nurse Practitioner-III (Competent) | Lactation Management, Normal Labor Care, Neonatal Resuscitation Training | PONEK (Comprehensive Emergency Neonatal Obstetrics Services) |
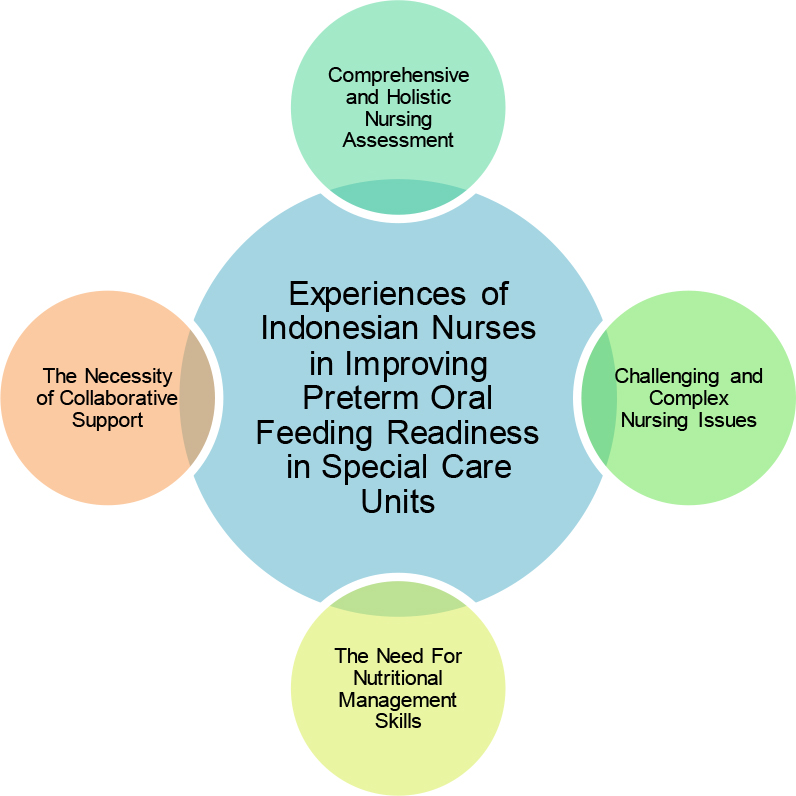
Four main themes were developed in this study, including 1) comprehensive and holistic nursing assessment, 2) challenging and complex nursing issues, 3) the need for nutritional management skills, and 4) the necessity of collaborative support (Figure 1).
Theme 1: Comprehensive and Holistic Nursing Assessment
The assessment of preterm infants’ readiness for oral feeding begins with an initial evaluation upon their admission to the intensive care unit. During this initial assessment, nurses consider various factors, including the infants’ general condition, gestational age, weight, breathing patterns, and primary complaints. For instance, preterm infants with favorable general conditions and stable breathing patterns are candidates for oral feeding. The assessment process is elucidated by the statements of the first and seventh participants:
“…the initial assessment will consider gestational age, weight, and the reason for admission…” (P1)
“…If the infant’s breathing pattern is compromised, we cannot use bottle feeding…” (P7)
Subsequently, an ongoing assessment is conducted, with the fourth participant emphasizing the importance of assessing the gastrointestinal tract’s function in preterm infants. This assessment involves examining factors such as gastric residue, intestinal sounds, the presence or absence of vomiting, and abdominal distension. Notably, gastric residue is evaluated by draining the feeding tube 1-2 hours before scheduled feedings rather than aspirating gastric fluid. This precautionary measure aims to minimize the risk of stress ulcers and necrotizing enterocolitis (NEC) in preterm infants.
“…if the residue is brown, it is the same as the yellow residue; if the stomach still shows optimal wall elasticity, we can feed the infant as long as the intestinal noise is positive…” (P4)
“…we do not use aspiration because it can cause stress ulcers and NEC…” (P4)
Data obtained from the assessment of gastrointestinal tract function serve as a basis for nurse evaluations, which include assessing the gastrointestinal tract’s absorption capacity, determining appropriate nutrient intake, and devising intervention plans for preterm infants. When breast milk is well-absorbed, nurses may increase the amount of breastfeeding or initiate sucking reflex stimulation. Conversely, if breast milk absorption is inadequate, the feeding interval may be extended. The third and fourth participants provide insights into this aspect:
“…usually, we look at the intake first. If the intake is good, preterm infants are given 10 ml of breast milk twice per shift. If this is good, it means it has good absorption. The infant can digest. When the infant shows this condition, we usually train the suction reflex…” (P3)
“…If an infant is given 3 cc and the residue during the day is recorded at 2 cc, it means there is a residue. With this condition, we extend the provision of nutrition from 3 hours to 4 to 5 hours…” (P4)
Additionally, the first participant highlights the significance of assessing the preterm infants’ ability to maintain physiological stability. Hemodynamic status, oxygenation, vital signs, and the type of oxygen therapy are assessed. If hemodynamic status and oxygenation are within normal limits, nurses proceed with oral feeding training, which may involve direct feeding, bottle feeding, or oral feeding during Kangaroo Mother Care (KMC):
“…for the nurse’s role in feeding, whether it’s bottle or oral, we check the infant first. If he is in good condition, with stable hemodynamics and breathing patterns, we then train the mother for oral feeding with KMC…” (P1)
It is essential to consider the type of oxygen therapy administered to preterm infants. Infants still reliant on invasive oxygen therapy, such as ventilators, should not undergo oral feeding. Enteral or parenteral feeding methods are alternatives for these infants. Only when preterm infants have transitioned to non-invasive oxygen therapy, such as nasal cannulas, can they participate in oral feeding exercises, as explained by the third participant:
“…If the infant’s condition improves, we prepare the infant for KMC, which is usually in the NICU here. The infant must be weaned from the ventilator. Maybe he is extubated if an endotracheal tube is attached or at least a Non-Invasive Ventilator (NIV) mask is attached…” (P3)
Moreover, the second and third participants introduce additional assessment steps for evaluating preterm infants’ oral-motor skills, focusing on their sucking and swallowing reflexes. This assessment involves observing feeding cues, assessing the strength and weakness of sucking and swallowing reflexes, and implementing assessment methods such as dripping breast milk through a syringe into the infants’ oral area or providing non-nutritive sucking using gauze soaked in glucose:
“…we check the suction reflex, sometimes we drip the infant’s mouth with breast milk…” (P2)
“…we then train the mother to use gauze or sterile cloths soaked in glucose, and then we observe the suction reflex…” (P3)
Theme 2: Challenging and Complex Nursing Issues
The data collected during the assessment phase served as the basis for identifying nursing problems in preterm infants experiencing oral feeding difficulties. Nurses followed nursing diagnosis formulation standards based on the Indonesian Nursing Diagnosis Standards (SDKI) and Indonesian Nursing Output Standards (SLKI). They analyzed the assessment data, comparing it with the definitions, causes, major data, and minor data specified in nursing standards. The tenth participant elaborated on this process:
“…first, let’s delve into the diagnosis-making process. We scrutinize the causes one by one, ensuring they align with SDKI and SLKI because our hospital adheres to them. We ensure that major symptoms and signs constitute about 80%, and then we establish the actual diagnosis, incorporating minor signs that bolster our diagnosis…” (P10)
The eighth participant pointed out that the most prevalent nursing problems encountered during the transition to oral feeding in preterm infants were related to nutritional deficits and the associated risk. These problems were linked to data indicating suboptimal nutrient absorption function, manifesting as red gastric residue, vomiting, abdominal distention, and weight loss:
“…nursing diagnoses can also manifest as a risk of nutritional deficit. Supporting data might include weight loss, the presence of feeding residue, vomiting, and ongoing abdominal distention” (P8)
Nutritional intake issues also stemmed from the oral-motor capabilities of preterm infants. The fifth participant described how nurses established a nursing diagnosis of ineffective breastfeeding, primarily based on the weak sucking and swallowing reflexes of preterm infants:
“…so, in specific cases, we might diagnose it as ineffective breastfeeding…” (P5)
Additionally, oral feeding readiness in preterm infants had an impact on their families. According to the eighth participant, nursing problems related to the ineffectiveness of lactation management could be identified in families with preterm infants. These issues included aspects such as the type of nutrition to be provided, breastfeeding methods, breast milk storage, the quantity of breastfeeding, and the timing of administration. This aligns with the statements of the seventh and eighth participants:
“…as for the family, the problem might pertain to lactation management…” (P8)
“…regarding milk feeding, whether it’s breast milk, expressed milk, or direct feeding, and how to store breast milk. If it’s formula milk, select the appropriate type of milk. These decisions fall to the family…” (P7)
Furthermore, nurses formulated nursing issues related to fluid intake. These problems emerged due to insufficient nutrient intake in preterm infants during the transitional phase of oral feeding and included issues such as hypovolemia:
“…if there’s a significant impact, reduced feeding naturally leads to reduced intake…” (P7)
Respiratory function in preterm infants also gave rise to nursing problems. This was linked to the immaturity of the respiratory system, resulting in disruptions to breathing patterns during oral feeding. These nursing issues were characterized by unstable hemodynamic status during oral feeding, including problems related to ineffective breathing patterns and airway clearance. Both types of nursing problems contributed to impaired oral feeding readiness in preterm infants, as described by the third participant:
“…in general, nursing problems in preterm infants with low birth weight often revolve around breathing patterns, particularly in cases where endotracheal tubes are employed for an extended period, airway hygiene frequently poses challenges…” (P3)
Theme 3: The Need for Nutritional Management Skills
Following the identification of nursing problems, nurses proceeded to implement interventions to enhance preterm oral feeding readiness. These interventions included various aspects, including nutritional management. The second participant described a practice where nurses addressed gastric residue issues. If the gastric residue appeared red, nurses either satisfied the preterm infant or performed gastric lavage:
“…if the infant is admitted with an orogastric tube in place, we check the residue. If possible, we may need to perform gastric lavage…” (P2)
The tenth participant highlighted the importance of assessing the color of stomach residues in preterm infants. When the residue was yellow, gradual feeding was continued. In specific cases, such as surgical instances involving preterm infants with gastroschisis, green residue prompted gradual feeding with dextrose or breast milk nutrition:
“…if the residue is only yellow, we can continue with small feedings. However, certain cases, particularly surgical cases like gastroschisis, may require fasting. But when the residue is green, the surgeon may recommend gradual feeding to stimulate the intestines, typically involving small increments. While formula milk is not advisable, dextrose or breast milk may be considered…” (P9)
Once the development of the gastrointestinal tract absorption function of preterm infants improved, nurses introduced trophic feeding. This gradual feeding approach, typically starting with 1-2 ml of breast milk per shift, aimed to stimulate the gastrointestinal tract’s function. It was aligned with the physiological characteristics of the infant’s small stomach, with the quantity of breastfeeding adjusted according to the infant’s weight. Participants provided insights into this practice:
“…we gradually introduce trophic feeding, starting at 1 cc for a few days, then progressing to 3 cc, and later 5 cc. We avoid immediately providing large amounts of feeding…” (P1)
“…Depending on the residue, if it appears clear and the stomach feels supple, we provide feeding as needed, in small increments. Infants have small stomachs, similar in size to peanut seeds. Trophic feeding involves gradual increases, with up to 1 cc, 2 cc, or 3 cc based on the infant’s requirements and weight…” (P4)
Furthermore, in the transition period of oral feeding for preterm infants, nurses actively stimulated the development of sucking and swallowing reflexes. They achieved this through non-nutritive sucking interventions, such as moistening gauze with dextrose and stimulating the infant’s mouth area to elicit sucking and swallowing responses. Once preterm infants had these reflexes, oral feeding exercises were initiated:
“…for stimulating the sucking reflex, we often employ gauze moistened with dextrose to elicit the reflex. We place it in the infant’s mouth, where we can hear the sucking sound. If the sucking reflex is present, we proceed with feeding, taking into account the infant’s ability to suck and swallow. Sometimes, an infant may have the sucking reflex but not the swallowing reflex, or vice versa…” (P4)
The fifth participant noted that oral feeding was initiated as soon as possible, provided there were no contraindications. Typically, oral feeding commenced when preterm infants reached a postmenstrual age of 34-35 weeks. The participant shared:
“…as long as it’s deemed appropriate for the infant to feed, we don’t delay the process. If there’s breast milk available, we use that for feeding…” (P5)
“…typically, oral feeding is initiated at a corrected age of around thirty-four to thirty-five weeks. If attempted earlier than this, the infant’s sucking reflex may be quite weak, and there’s a risk that the infant could choke, as breast milk may still flow too easily…” (P5)
However, the fourth participant emphasized that the initiation of oral feeding didn’t necessarily depend on reaching a specific corrected age, such as 34 or 36 weeks. Instead, it hinged on the infant demonstrating a proficient sucking reflex. This approach allowed nurses to start oral feeding for preterm infants once they had this capability:
“…it doesn’t have to be precisely at 34 or 36 weeks of gestation; that’s not a strict requirement. Essentially, if the infant demonstrates a strong sucking reflex, we begin feeding. We don’t fixate on specific gestational ages, like 32 or 33 weeks…” (P4)
Nurses evaluated the progress of preterm infants’ oral feeding readiness throughout the oral feeding period. Evaluations performed during each shift included assessments of gastric residues, gastrointestinal bleeding, abdominal distention, and intestinal noise. To maintain continuity of documentation, nurses recorded the oral feeding progress of preterm infants in electronic medical records:
“…typically, with each shift, we assess the suction, feeding, and gastric residue reflexes. During these assessments, we monitor for any signs of distension or gastrointestinal bleeding. If everything appears favorable, we continue to observe, provided there are no contraindications. We reevaluate, checking for good bowel sounds, absence of residue, and non-distended conditions before proceeding with intake…” (P3)
Additionally, the second and tenth participants mentioned conducting further evaluations by examining anthropometry and nutritional status, particularly weight gain, when there was an improvement in the sucking reflex:
“…we manage the nutrition and then conduct body weight measurements and assess fluid balance…” (P2)
“…anthropometry is crucial. We measure weight to determine if it aligns with our expectations. We also pay attention to the status of the sucking reflex, whether it’s improving or deteriorating…” (P10)
Theme 4: The Necessity of Collaborative Support
The participants engaged in collaborations with other healthcare professionals to enhance the readiness of preterm infants for oral feeding, including pediatricians. This collaboration involved considerations regarding the timing and method of oral feeding. Additionally, there was a collaboration in administering medication therapy to minimize gastrointestinal bleeding, such as vitamin K and erythromycin.
“……..he also advised to give oral intake gradually…” (P2)
“… medical action, for example, gastric bleeding can be given vitamin K or erythromycin…” (P8)
In cases where some preterm infants struggled with the transition to oral feeding, as indicated by suboptimal weight gain, the sixth participant emphasized the importance of nurses collaborating further with the metabolic nutrition division. Recommendations made to the metabolic nutrition division included providing enteral nutrition for maintenance.
“… usually, the infants are fed three to four times per shift by being trained by drip via an orogastric tube, and then we train them to feed via bottle, too. If the infant’s weight is not optimal or his oral nutritional performance is not good, a metabolic nutrition specialist will replace it with formula milk. We then perform maintenance, so for 8 hours, for example, we feed the infant per hour, and then we evaluate whether there’s residue or not. We can feed for 4 hours straight or 5 hours depending on the body weight…” (P6)
The first participant mentioned another form of collaboration involving working with the medical rehabilitation department to train the sucking and swallowing reflexes of preterm infants. These exercises, known as oro-motor training, aim to enhance preterm infants’ oral feeding readiness.
“…so far, preterm infants need good suction reflex though it is difficult. We train preterm infants to have it. We often work with the Medical Rehabilitation department to do oro-motor training…” (P1)
The participants also highlighted the importance of collaborating and partnering with families to enhance the oral feeding readiness of preterm infants. They motivated families to optimize breastfeeding in the intensive care room, as it is beneficial for the development of preterm infants’ gastrointestinal tracts. Nurses provided education on breastfeeding techniques and Kangaroo Mother Care (KMC) to support the oral feeding of preterm infants.
“…we provide education when patients are still being treated here in the hope that when the mother’s milk comes out, we recommend breast milk only. We also educate on how to express breast milk that can be stored in breast milk bags…” (P2)
“…we provide education to mothers on how to express breast milk…” (P5)
Discussion
This study addresses the research objective of exploring nurses’ experiences enhancing oral feeding readiness in caring for preterm infants within the special care unit. The study has identified four main themes, which are discussed below.
The first theme, “Comprehensive and Holistic Nursing Assessment,” indicates how nurses assess preterm infants’ oral feeding readiness in special care units. The assessment process consists of both initial and follow-up evaluations. The initial assessment includes an evaluation of the overall condition, including gestational age, birth weight, and primary complaints. Evaluating gestational age and birth weight is vital as they are linked to the infant’s ability to develop oral feeding skills (Alshaikh et al., 2022; Kamity et al., 2021). Subsequently, nurses conduct follow-up assessments to monitor the gastrointestinal tract’s functioning. This involves selectively checking for gastric residue without employing negative pressure, which could potentially harm the gastric mucosa and lead to the loss of digestive enzymes (Elia et al., 2022; Williams et al., 2023). Additional assessments include the evaluation of oxygenation status and oral motor skills. This includes assessing sucking reflexes, swallowing reflexes, sucking-swallowing-breathing coordination, the risk of aspiration, hypoxia, the physiological status of preterm infants, and increased energy expenditure (Azuma & Maron, 2020).
A comprehensive nursing assessment also involves evaluating the oral feeding readiness behavior of preterm infants. Astuti et al. (2022) emphasize the importance of assessing behavioral cues, such as oral feeding, in preterm infants during nursing assessments. Nurses can implement the Synactive Theory of Development Model to aid the assessment process. This model outlines the communication relationship between various subsystems, including physiological stability, motor systems, behavior regulation, interaction or attention, and self-regulation. Behavioral subsystem assessments may involve observing whether the baby actively makes eye contact with the caregiver, observing hand positioning towards the mouth or face, and monitoring midline positioning (Browne, 2021). Nurses may also employ assessment instruments that apply a cues-based feeding approach, such as the Early Feeding Skills (EFS) instrument. The EFS instrument evaluates preterm infants’ oral feeding readiness behavior before, during, and after feeding, allowing for a comprehensive assessment of their feeding capabilities (Kamran et al., 2023).
The second theme, “Challenging and Complex Nursing Issues,” was encountered during the oral feeding transition period for preterm infants. These nursing challenges include respiratory function, nutrition, and the role of parents.
Respiratory issues stem from the immaturity of the pharyngeal phase, placing preterm infants at risk of impaired sucking-swallowing-breathing coordination, leading to gastroesophageal reflux disease (GERD). This condition results from disorders in the esophageal mechanism, chemoreceptors, osmoreceptors, and esophageal dysmotility (Hasenstab & Jadcherla, 2022). Nutrition-related problems arise due to the immaturity of the gastrointestinal tract, leading to impaired nutrient absorption and an increased risk of extrauterine growth restriction (EUGR) in preterm infants (Peila et al., 2020). Research by Xiang et al. (2021) in intensive care units revealed that 75% of very preterm infants experienced EUGR upon discharge, with Fenton chart assessments falling below the 10th percentile and a mean weight age z-score (WAZ) value of -2.41 standard deviations.
Mothers of preterm infants with oral feeding difficulties encounter significant psychological challenges, including increased stress, anxiety, and reduced confidence in providing oral feeding. These challenges manifest when infants have weak sucking reflexes or require gastric tube feeding (Chapko et al., 2022; Morelius et al., 2020). Mothers’ insufficient knowledge and skills in providing oral feeding to preterm infants contribute to these problems (Isazadeh et al., 2022), impacting the physical and mental dimensions of their quality of life (Kamran et al., 2023).
The third theme, “The Need for Skills in Nutritional Management,” indicated that nurses must possess specific skills in analyzing gastric residue in preterm infants. The evaluation of gastric residue serves the critical purpose of assessing the incidence of NEC, an emergency condition in preterm infant care (Williams et al., 2023). Notably, hemorrhagic and green gastric residues correlate significantly with NEC diagnosis within 24 hours (Purohit et al., 2021). Hemorrhagic gastric residue may indicate mucosal injury due to aspiration during examination or the presence of an endotracheal tube (Purohit et al., 2021). Furthermore, nurses must consider dark green gastric residue, indicating the presence of bile acids that activate key digestive molecules and receptors like farnesoid-X-receptor (FXR) and G protein-coupled bile acid receptor 1 (GPBAR1/TGR5) (Elia et al., 2022).
Another essential nutritional management skill for nurses is the ability to administer gradual oral feeding or trophic feeding. Trophic feeding, initiated with 1–2 mL/kg/dose or 10-15ml/kg/day, begins early in a preterm infant’s life. It promotes gastrointestinal system development, enhances feeding tolerance, accelerates weight gain, and reduces the risk of sepsis (Galal et al., 2023; Kebede et al., 2022). Research by El Houchi et al. (2022) emphasizes that trophic feeding with breast milk or colostrum significantly lowers the incidence of NEC and sepsis in preterm infants. Improving nurses’ knowledge of trophic feeding practices is essential to enhance preterm infant care outcomes (Galal et al., 2023).
Additionally, nurses require expertise in developmental stimulation to enhance oral feeding readiness, commencing with NNS when preterm infants develop sucking and swallowing reflexes at postmenstrual age 28-33 weeks (Viswanathan & Jadcherla, 2020). Developmental stimulation includes dripping breast milk into the oral area to provide positive oral experiences simulating the sensory experiences of amniotic fluid in the intrauterine environment (Orourke et al., 2023). Another effective nursing intervention is non-nutritive sucking using gauze soaked in dextrose. Research indicates this intervention improves oral feeding outcomes, reducing abdominal distension and vomiting (Gutiérrez et al., 2022). Combining non-nutritive sucking with dextrose creates a synergistic effect, promoting oral-tactile stimulation and the release of serotonin and endorphins, contributing to the infant’s comfort (García-Valdivieso et al., 2023).
The fourth theme highlights the “Necessity for Collaborative Support” in enhancing preterm oral feeding readiness. Nurses engage in collaboration with various professionals to provide comprehensive care for preterm infants. One form of collaboration involves fostering solid partnerships between neonatal nurses, medical rehabilitation specialist doctors, and physiotherapists (Shon et al., 2021). The interprofessional approach includes individual professional competence, teamwork, and achieving optimal goals. Nurses are pivotal in promoting teamwork and effective communication, such as working together to provide oral-motor stimulation for preterm infants (Haemmerli et al., 2021; Shon et al., 2021).
Additionally, collaboration extends to working closely with parents and families to enhance preterm infants’ readiness for oral feeding. The family environment significantly influences this readiness, and the FCC approach emphasizes parental involvement. FCC principles include information exchange, respect for differences, building relationships, collaboration, and negotiation within the family context. Collaboration between nurses and families involves the educational process and the implementation of KMC. The FCC approach enhances parents’ knowledge and skills, empowering them to confidently care for their infants under nursing supervision (Lorié et al., 2021; Morelius et al., 2020).
Strengths and Limitations of the Study
This research has comprehensively explored nurses’ experiences in enhancing preterm oral feeding readiness in both Level III and Level II intensive care units. This exploration was conducted through in-depth interviews and the examination of nursing record documentation. However, a limitation of this study was the absence of further investigation from multidisciplinary perspectives, including doctors, physiotherapists, and speech therapists. Therefore, it is recommended that future research should explore preterm oral feeding readiness from a multidisciplinary standpoint.
Implications of the Study
This research has significant implications for nursing, particularly for neonatology nurses caring for preterm infants in special care units. These nurses should focus on developing specialized skills to enhance preterm oral feeding readiness. These essential skills include conducting comprehensive assessments and evaluating the physiological functions of preterm infants’ body systems, such as the neuromuscular and gastrointestinal tract. Additionally, nurses should excel in behavioral assessments, keenly observing preterm infants’ oral feeding readiness cues. Addressing nursing challenges related to preterm infants’ oral feeding abilities, such as coordinating sucking-swallowing-breathing and managing the psychological impact on parents, particularly maternal stress, is paramount.
Furthermore, nurses must possess proficiency in nutritional management, including the skills required for analyzing gastric residues in preterm infants, delivering trophic feeding, and stimulating development to boost oral feeding readiness. Innovative nursing interventions, such as gently introducing breast milk to the oral area of preterm infants to provide a positive oral experience, are essential. Collaborative skills are equally vital for neonatology nurses. They should cultivate cooperative relationships with other healthcare professionals, including doctors, physiotherapists, and speech therapists. Moreover, nurses should engage in effective partnerships with families to implement nursing interventions to enhance preterm oral feeding readiness through education and KMC practices.
Conclusion
Preterm infants necessitate thorough nursing care to enhance their readiness for oral feeding. Nurses should conduct a comprehensive and holistic assessment, including evaluating physiological functions such as the gastrointestinal tract and the maturity of primitive reflexes, alongside assessing preterm infants’ feeding behavior. The transition from enteral to oral feeding presents complex nursing challenges for preterm infants, demanding that nurses enhance their skills in nutritional management to improve oral feeding capabilities. Effective stimulation is essential to boost oral feeding readiness, necessitating multidisciplinary collaboration and collaboration with families. This research is a basis for developing an intervention model to enhance preterm oral feeding readiness.