Background
After coronary artery bypass graft (CABG) surgery, patients have sternal and saphenous vein graft (SVG) donor site wounds, which limit their movement due to the multiple wound sites and sizes, especially regarding the SVG donor site wound. These wounds influence the patient’s ability to perform self-care during the postoperative recovery period. CABG patients are also concerned about surgical wound care after discharge from the hospital because the wound may become infected if it does not receive adequate care (Lie et al., 2012; Oshvandi et al., 2020).
Wound healing in patients with CABG is considered primary intention healing, with the edges of the wound pulled together via suturing. Although the wound usually heals within 21 days or three weeks (Annesley, 2019), wound healing is relatively slower in patients with diabetes (Patel et al., 2019). Of patients undergoing CABG, 40% have a history of diabetes (Gull et al., 2018). Hyperglycemia is correlated with slow wound healing. Among patients with uncontrolled diabetes, wound healing is slower, which increases the risk of surgical site infections (SSIs) development (Delmore et al., 2017; Duggan et al., 2017; Nabngarm et al., 2015). SSIs in patients after CABG, on average, occur after discharge from the hospital, mostly within the first two weeks or on days 14–21 after surgery (Logan et al., 2016; Rochon et al., 2018).
A previous study on patients with CABG reported that incidence rates of SSIs in sternal and SVG donor site wounds after hospital discharge were 49.4% and 72.6% (Si et al., 2014). These results are consistent with the findings of Sanonoi et al. (2021), who found that patients with CABG and co-morbid diabetes had been hospitalized within 28 days after hospital discharge due to SSIs, 25% of which occurred in SVG donor site wounds. Most patients with CABG have a history of diabetes, a significant predictor of SSIs after CABG surgeries, and causes delayed wound healing (AlRiyami et al., 2022).
Patients with CABG usually receive discharge planning detailing the medicine used and recovery process; however, this does not include information related to the continuity of home care for surgical wounds after discharge from the hospital. Most patients lacked knowledge and skills in observing the wound for any abnormal signs and symptoms, wound care, or consuming healthy foods that could help their wounds to heal faster, as patients have insufficient knowledge or cannot remember the advice (Atinyagrika Adugbire & Aziato, 2018). Moreover, patients have uncontrolled diabetes. These may be the factors causing SSIs, which result in slow wound healing, poor postoperative recovery, the inability to perform self-care in daily activities, and patients being unable to resume their work. The latter can lead to reduced family income. These consequences can also have an impact on a patient’s physical and mental status, resulting in decreased quality of life (Sanger et al., 2014; Tanner et al., 2012).
Currently, patient health monitoring using telehealth has progressed markedly. Telehealth is a tool that uses information and communication technology for health care, including the transmission of health information between patients and healthcare providers. Previous studies (Ruttanamontree et al., 2020; Somsiri et al., 2021; Yuroong et al., 2021) have used telehealth to track patients awaiting surgery and after surgery, which improves patients’ functional status and reduces the rate of hospitalization and anxiety. Using telehealth for wound monitoring, mostly chronic wounds, resulted in better wound healing (Goh & Zhu, 2017). Only a small number of studies have followed surgical incisions after hospital discharge. In patients undergoing vascular surgery, abnormalities or signs of SSI were detected (Gunter et al., 2018; Mousa et al., 2019).
However, recent studies have not been able to promote wound healing and monitoring in patients with diabetes undergoing CABG continuously while both admitted to the hospital and after discharge. Therefore, our study aimed to investigate the effects of the telehealth program for wound healing promotion (TPWHP) on wound healing of sternal and SVG donor site wounds in patients with diabetes undergoing CABG.
Methods
Study Design
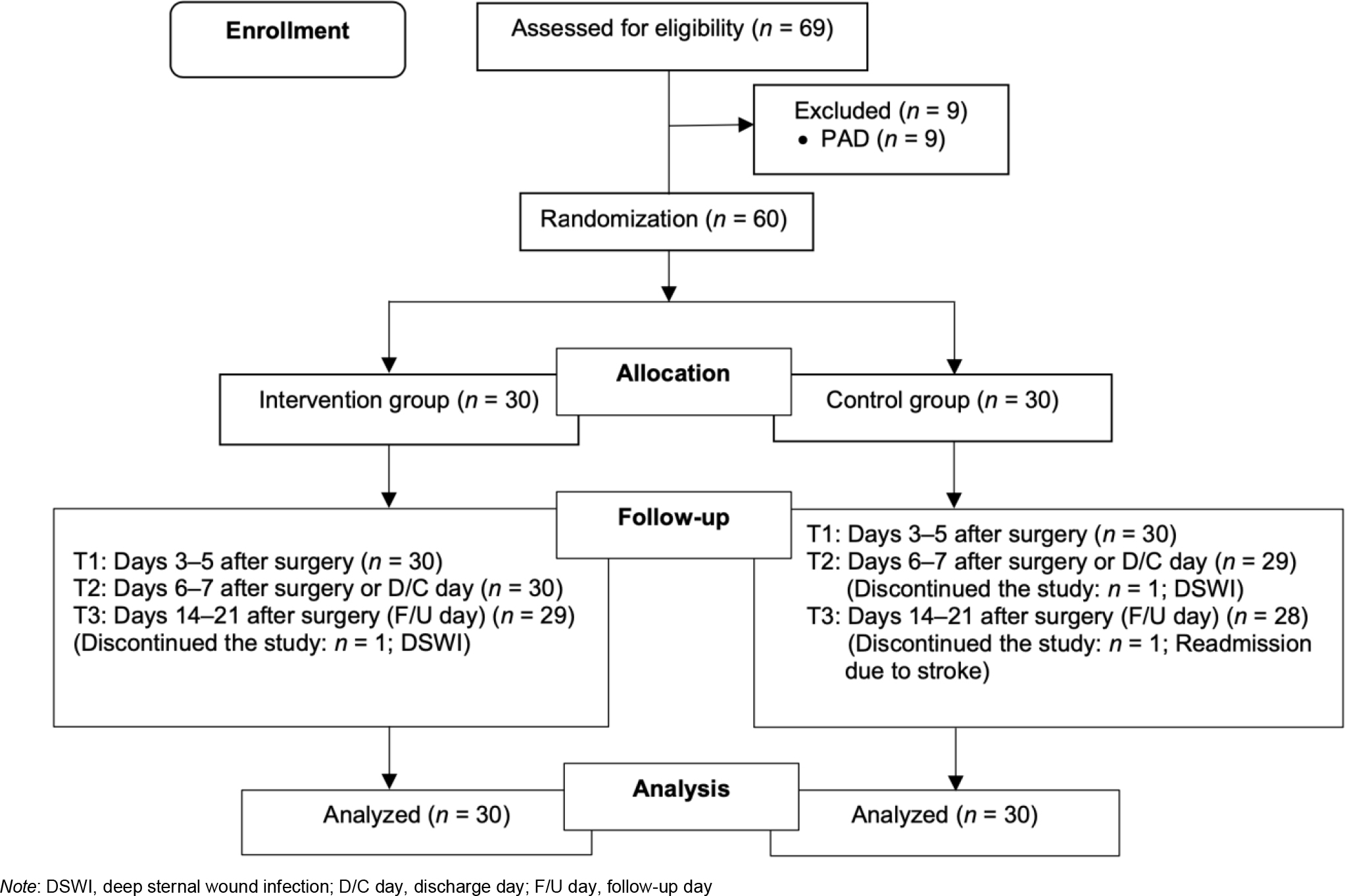
This parallel, randomized controlled trial was performed in accordance with CONSORT guidelines (Schulz et al., 2010). Participants were randomly allocated into an intervention group (TPWHP plus routine nursing care) or a control group (routine care only). A blind assessor was concealed by the research assistants as the evaluator.
Samples/Participants
This study was conducted at two university hospitals in Bangkok, Thailand, from June 2020 to November 2020. The researchers selected these two university hospitals because they had the highest number of CABG surgeries in Thailand. The participants comprised female and male patients with diabetes, aged ≥18 years, who had undergone CABG. The inclusion criteria were as follows: a) a history of type 2 diabetes or fasting blood glucose ≥126 mg/dL or random blood glucose ≥200 mg/dL; b) a history of elective CABG surgery alone or CABG in combination with other open-heart surgeries for the first time; c) an access to a smartphone and internet connection; and d) literacy in the Thai language. The exclusion criteria were as follows: a) a diagnosis of peripheral arterial disease or absence of a palpable pulse in the dorsalis pedis or posterior tibial artery (grade 0), and b) a history of cognitive impairment according to criteria of the Thai Mental State Examination (TMSE scores <24) for patients aged >60 years. The discontinuation criteria were as follows: a) had undergone reoperation, cardiopulmonary resuscitation, and readmission after discharge; b) being unable to contact patients in the intervention group twice after discharge; and c) having a length of hospital stay of >10 days due to postoperative complications, including postoperative atrial fibrillation, pulmonary congestion, acute renal failure, cerebral ischemia, and deep incisional or organ/space SSI requiring removal of surgical sutures to debridement, and having infections in various body systems.
The sample size was calculated by power analysis. The effect size from a similar study by Dumfarth et al. (2008) was 0.86, calculated by G* Power 3.1, with the power of the test value set at 0.80 and the statistical significance level at 0.05. A two-tailed test hypothesis and an independent t-test were performed to calculate the sample size. Twenty-three samples were required per group, and the number of samples was increased to 30% to prevent attrition, referring to the attrition rate from a similar study by Musa et al. (2018); thus, 30 samples per group were required for a total of 60 samples. The enrolled patients were randomly assigned to the following groups from two university hospitals with an equal number of intervention and control groups in a ratio of 1:1 utilizing a simple random sampling method that used a computerized random number generator (Figure 1). Both hospitals had 15 samples each in the intervention and control groups. The researcher and research assistants met with the participants in a private area to prevent sample contamination.
Instruments
Two instruments were used for the data collection. The content validity tests of these instruments were performed by three experts: a cardiothoracic surgeon, a nurse instructor, and a cardiothoracic surgery nurse. Data were collected using a demographic and health-related data form and the Thai wound assessment inventory (WAI) developed by Holden lund (1988), which was translated into Thai by Nabngarm et al. (2015). The researchers asked permission for the use of the tool in this study. The assessment included observation of three wound characteristics: 1) edema, 2) erythema, and 3) exudate. Each characteristic was scored using a 4-point scale: 0, none; 1, few; 2, intermediate; and 3, high. The total score for each characteristic ranged from 0 to 9, divided by 3, obtaining scores between 0 and 3. The scores were interpreted as follows: a lower score indicated good wound healing according to the wound healing process. A higher score indicated a high degree of wound inflammation or slow wound healing. The WAI in a previous study obtained an inter-rater reliability of 0.70 (Holden lund, 1988). For this study, the researcher assessed the tool together with the research assistants by performing a test involving ten patients with diabetes undergoing CABG who shared the same characteristics. The assessment results were calculated for the inter-rater reliability, which was 0.91 (95% CI 0.62–0.98). This tool had a content validity index of 1.0.
Interventions
Both groups received routine nursing care in the cardiovascular and thoracic surgery wards of the two university hospitals, which have similar guidelines for surgical wound care and prevention of surgical wound infections. The control group received routine nursing care through verbal instruction, including cleaning the body preoperatively, medication administration, intake of healthy food to control blood glucose, cardiac rehabilitation, surgical wound care, signs and symptoms of SSIs, and distribution of a practical manual with the contents of the corresponding manual depending on the hospital where the patients undergoing CABG were being treated. In addition, the control group received dietary care for patients with diabetes and medications to control blood glucose according to the treatment plan. For surgical wound care, during hospitalization, in the absence of fluid drainage from the wound, the wound was covered with gauze for 72 h, the wound was cleaned, and the dressing was changed for the first time on postoperative days 3–5 and the second time on postoperative days 6 and 7 or the date of hospital discharge. The wound was covered with wound dressing until the follow-up day after discharge at 1–2 weeks.
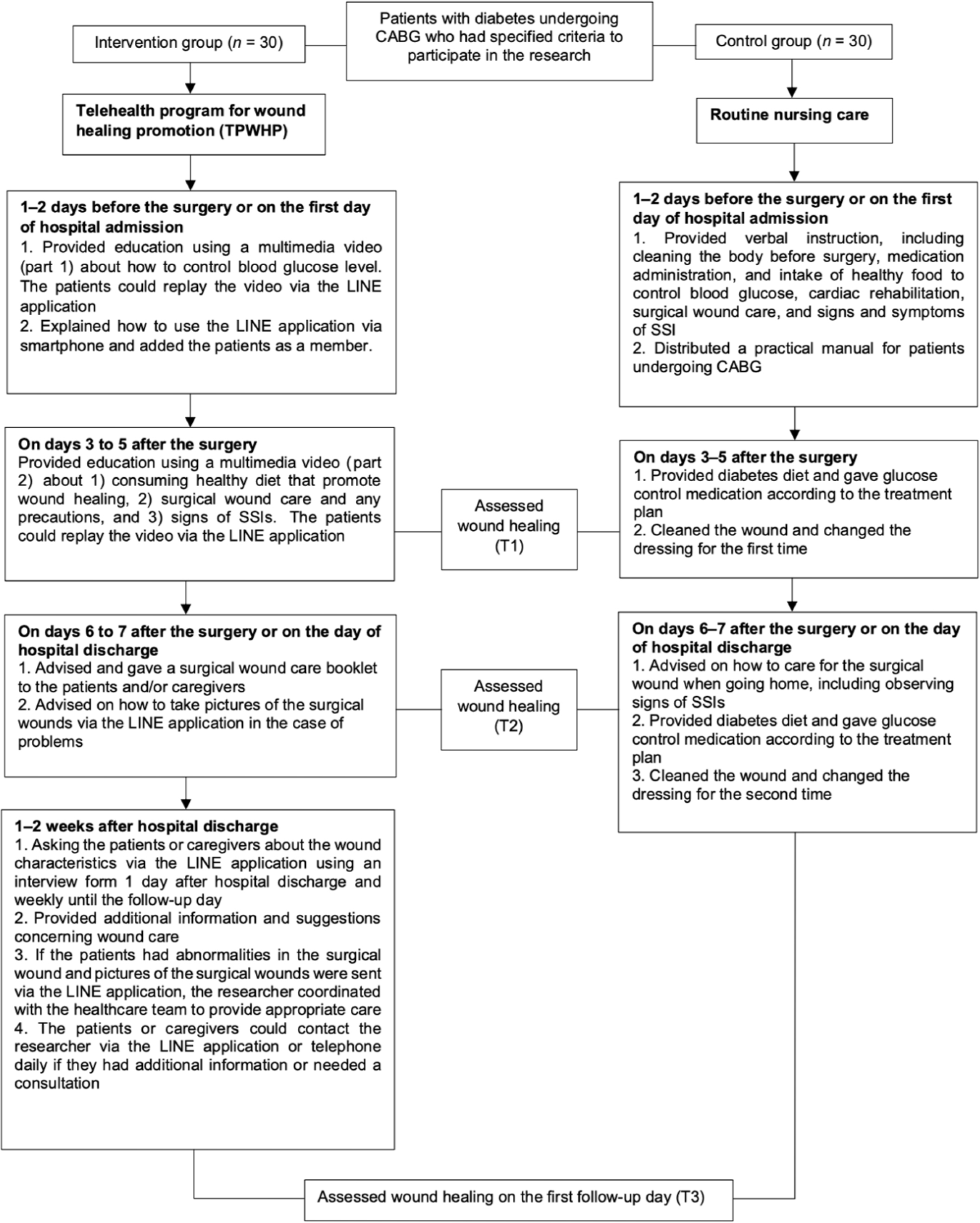
The intervention group received routine nursing care along with the TPWHP provided by the researchers. The TPWHP was created based on Neuman’s Systems Theory (Neuman & Fawcett, 2011), which includes the prevention of stressors affecting wound healing using knowledge of wound assessment and prevention, risk and symptom management, and a literature review on wound healing and surgical wound care specifically after CABG surgery. The program promoted wound healing and continuity of care throughout the 1–2-week period after hospital discharge via the LINE application on a smartphone, a communication application that the majority of Thai people can access and commonly used in Thailand. Figure 2 presents the flow and detail of the TPWHP intervention, which had been divided into two phases.
In phase 1, which was during hospital admission, specifically 1–2 days before the surgery or on the first day of hospital admission, the researcher provided education using a video (part 1) about how to control blood glucose levels. This required approximately 3 minutes. The researcher then added the patient as a friend to the application and explained the communication procedures and wound monitoring via the LINE application on a smartphone. On postoperative days 3–5, information on diet, helping with wound healing, surgical wound care, precautions, and signs of SSI was given using part 2 of the video. This part took nearly 7 minutes to complete. The patients could replay the video via the LINE application. On days 6–7 after the surgery or on the day of hospital discharge, a surgical wound care booklet was given to the patients and/or caregivers. They were given wound care interventions to do at home in case exudates were present, the wound dressing was damp or wet, or the dressing was peeling or itchy. The patients and caregivers were also advised on how to take pictures of the surgical wounds and send them via the LINE application in case of problems with the wounds requiring additional assessment and care.
During phase 2, which was the period of 1–2 weeks after hospital discharge, the researcher evaluated the surgical wound by asking patients about the wound characteristics via the LINE application using an interview form for surgical wound follow-up. This was performed on the first day after hospital discharge and weekly until a follow-up outpatient appointment. The researcher also provided additional information and suggestions concerning wound care. The researcher used a telephone to contact patients that did not respond via the LINE application more than two times. The patients or caregivers could contact the researcher via the LINE application or telephone daily from 8:00 AM to 8:00 PM if they had additional information or needed a consultation regarding the intervention.
The patients and caregivers could take pictures of the surgical wounds and send them via the LINE application in the event that the patients had abnormalities in the surgical wound, such as swelling around the wound, redness, heat, or exudates in conjunction with increased pain and tenderness around the wound. The researcher coordinated with the health care team. For this research, the researcher established a team of doctors and nurses from each hospital as consultants and patient information to ensure the provision of appropriate care.
Data Collection
Patients with diabetes undergoing CABG were approached at the cardiovascular and thoracic surgery wards of the two university hospitals and screened for eligibility by registered nurses in the wards. If they were interested in participating in the study, the nurses introduced the researcher to them. The researcher invited patients with diabetes undergoing CABG who met the study criteria to participate in this study. The researcher collected the personal data of all participants.
The research assistants, who were nurses trained by the researcher in data collection outcomes, collected the following outcomes: wound healing status of both sternal and SVG donor sites at T1 on days 3–5 after surgery as preliminary information, T2 on days 6–7 after surgery as the day of hospital discharge, and T3 on days 14–21 after surgery as the follow-up day in the outpatient department. The research assistants assessed the wounds during wound care and dressing changes. During assessment in both the intervention and control groups, the research assistants took pictures of the wounds to monitor wound healing. The photos were used only for the study and would not be published without permission.
Data Analysis
All data were analyzed using the SPSS statistical program for Windows version 18.0. Intention-to-treat analysis was used in this study. Descriptive statistics were used to analyze the participants’ characteristics. The Chi-squared and Fisher’s exact tests were used to determine the differences in the participants’ characteristics between the two groups. Due to the abnormal distribution, the Mann–Whitney U test was used for comparing the mean rank score differences in sternal and SVG donor site wound healing between the two groups.
Ethical Considerations
This research project was approved by the Human Research Protection Committee in the Faculty of Medicine Siriraj Hospital, Mahidol University (COA No. Si 270/2020) and the Faculty of Medicine Chulalongkorn University (COA No. 538/2020) and registered with the Thai Clinical Trials Registry (TCTR20211112002). All participants were informed about the objectives of the research project, data collection, procedures, expected benefits, and potential risks. The participants could withdraw from the study until data collection was concluded, and their withdrawal would not affect their treatment or care received. In addition, all participants signed the consent forms, fostering trust and research integrity.
Results
Demographic and Health-Related Data
The baseline demographic and health-related data were not significantly different between the intervention and control groups (p >0.05) (Table 1). Most of the participants in both groups were male (80%). Half of the participants in both groups had a history of diabetes of >10 years. The intervention and control groups had a mean age of 66.5 ± 9.4 and 67.4 ± 9.9 years, respectively. The intervention and control groups had mean body mass index (BMI) of 25.8 ± 3.8 and 25.7 ± 5.1 kg/m2, respectively.
| Characteristics | Intervention group (n = 30) | Control group (n = 30) | Total (n = 60) | p-value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Gender | ||||
| Male | 24 (80) | 24 (80) | 48 (80) | 1.000b |
| Female | 6 (20) | 6 (20) | 12 (20) | |
| Age (years), mean ± SD | 66.5 ± 9.4 | 67.4 ± 9.9 | 67 ± 9.6 | 0.729a |
| BMI (kg/m2), mean ± SD | 25.8 ± 3.8 | 25.7 ± 5.1 | 25.8 ± 4.5 | 0.910a |
| Duration of diabetes | ||||
| <1 year | 3 (10) | 5 (16.6) | 8 (13.3) | 0.334c |
| 1–5 years | 10 (33.3) | 5 (16.7) | 15 (25) | |
| 6–10 years | 2 (6.7) | 5 (16.7) | 7 (11.7) | |
| >10 years | 15 (50) | 15 (50) | 30 (50) | |
| Diabetes medications | ||||
| None | 4 (13.3) | 3 (10) | 7 (11.6) | 1.000c |
| Oral medication | 21 (70) | 21 (70) | 42 (70) | |
| Insulin | 2 (6.7) | 2 (6.7) | 4 (6.7) | |
| Oral medication + insulin | 3 (10) | 4 (13.3) | 7 (11.7) | |
| Suturing | ||||
| Subcuticular suture | 30 (100) | 28 (93.3) | 58 (96.7) | 0.492c |
| Staple | 0 (0) | 2 (6.7) | 2 (3.3) | |
| Length of SVG donor wound | ||||
| Below knee to ankle | 9 (30) | 14 (46.7) | 23 (38.3) | 0.184b |
| Thigh to ankle | 21 (70) | 16 (53.3) | 37 (61.7) | |
| HbA1C (mg%), mean ± SD | 7.6 ± 2.2 | 7.2 ± 1.6 | 7.4 ± 1.9 | 0.483a |
| Blood glucose (mg/dL), mean ± SD | ||||
| Preoperative* | 151.4 ± 65.5 | 141.4 ± 46.5 | 146.4 ± 56.5 | 0.495a |
| Postoperative** | ||||
| - Day 1 (24 h) | 215.3 ± 45.1 | 194.9 ± 39.1 | 205.1 ± 43.1 | 0.066a |
| - Day 2 (48 h) | 199.2 ± 55.8 | 176.8 ± 42.6 | 188 ± 50.5 | 0.085a |
| - Day 3 (72 h) | 183.3 ± 46.8 | 165.3 ± 39.7 | 174.3 ± 44 | 0.111a |
| - Day 14-21 (F/U day)* | 132.5 ± 29.3 | 149.1 ± 36.5 | 140.7 ± 33.8 | 0.068a |
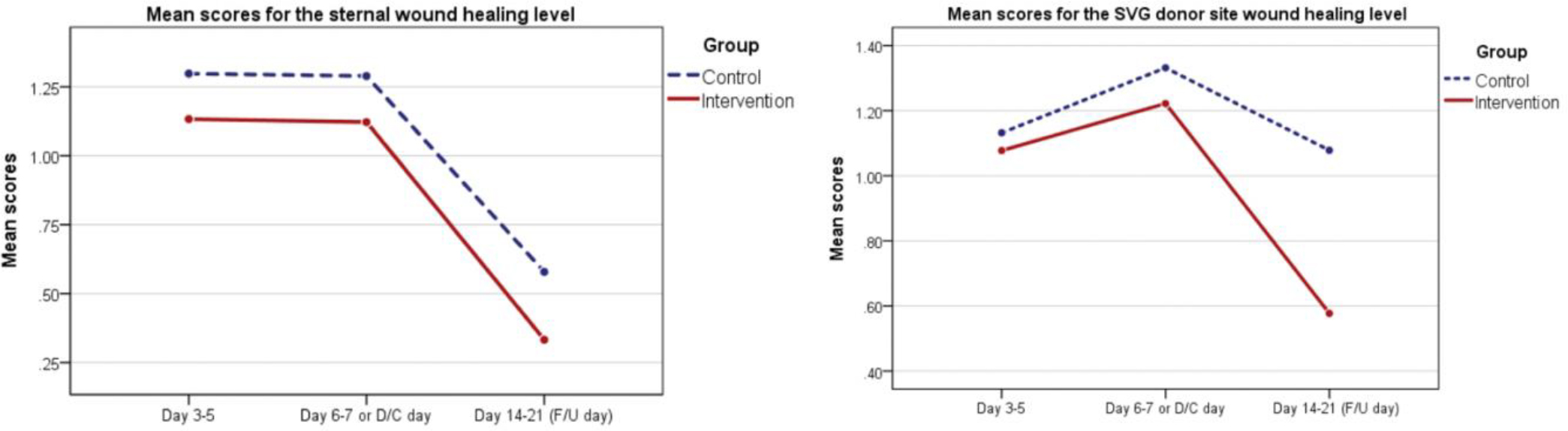
Sternal Wound Healing
Table 2 shows the mean and mean rank scores for the sternal wound healing level between the intervention and control groups. The data did not have a normal distribution, so nonparametric statistics were used. The mean rank scores for the sternal wound healing level on T3 were not statistically different between the intervention and control groups (p = 0.126); however, the intervention group showed lower mean scores than the control group (mean = 0.33 ± 0.46 and 0.58 ± 0.67, respectively).
| Time | Intervention group | Control group | Z | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | Median (IQR) | Mean Rank | n | Mean ± SD | Median (IQR) | Mean Rank | |||
| Day 3–5 (T1) | 30 | 1.13 ± 0.24 | 1.00 (0.33) | 27.25 | 30 | 1.30 ± 0.44 | 1.32 (0.33) | 33.75 | -1.602 | 0.109 |
| Day 6–7 (D/C day) (T2) | 30 | 1.12 ± 0.27 | 1.00 (0.00) | 27.38 | 30 | 1.29 ± 0.44 | 1.00 (0.67) | 33.62 | -1.712 | 0.087 |
| Day 14–21 (F/U day (T3) | 30 | 0.33 ± 0.46 | 0.33 (0.42) | 27.23 | 30 | 0.58 ± 0.67 | 0.67 (0.67) | 33.77 | -1.531 | 0.126 |
Note: D/C = Discharge, F/U = Follow-up | significant at p <0.05, p-value from Mann–Whitney U test | A lower score means a good level of wound healing
SVG Donor Site Wound Healing
Table 3 shows the mean and mean rank scores for the SVG donor site wound healing between the intervention and control groups. The mean rank scores for the SVG donor site wound healing level on T3 were statistically different between the two groups (p = 0.012). The intervention group had lower mean scores than the control group (mean = 0.58 ± 0.54 and 1.08 ± 0.82, respectively), with the intervention group showing SVG donor site wound healing better than the control group (see Figure 3).
| Time | Intervention Group | Control Group | Z | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | Median (IQR) | Mean Rank | n | Mean ± SD | Median (IQR) | Mean Rank | |||
| Day 3-5 (T1) | 30 | 1.08 ± 0.21 | 1.00 (0.33) | 28.10 | 30 | 1.13 ± 0.16 | 1.00 (0.33) | 32.90 | -1.259 | 0.208 |
| Day 6-7 (D/C day) (T2) | 30 | 1.22 ± 0.31 | 1.00 (0.33) | 27.27 | 30 | 1.33 ± 0.30 | 1.33 (0.33) | 33.73 | -1.538 | 0.124 |
| Day 14-21 (F/U day) (T3) | 30 | 0.58 ± 0.54 | 0.33 (0.34) | 24.90 | 30 | 1.08 ± 0.82 | 1.00 (1.34) | 36.10 | -2.526 | 0.012* |
Note: D/C = discharge, F/U = follow-up |
A lower score means a good level of wound healing
Discussion
The findings demonstrated the effectiveness of the TPWHP on wound healing among patients with diabetes undergoing CABG. TPWHP includes wound monitoring in the hospital and after hospital discharge. This program was conceptualized using the Neuman systems theory. The program consisted of the primary, secondary, and tertiary prevention stages, which prevented the patients from experiencing stressors that could affect wound healing (Neuman & Fawcett, 2011).
The primary prevention stage (first stage) aimed to educate patients with CABG or their caregivers in acquiring knowledge, understanding, and practicing appropriate measures to prevent stressors or reduce risk factors. This stage also included the information and knowledge using multimedia since the patients were admitted to the hospital, and their wounds were monitored via the LINE application after hospital discharge. Consistent with the results of a previous study, providing knowledge on surgical wound care through multimedia before hospital discharge was effective, empowering patients with knowledge and skills to care for their wounds effectively (Jimenez et al., 2021; Tu et al., 2012).
After hospital discharge, the researcher monitored the conditions of the surgical wound via the LINE application. In the intervention group, one case of an SVG donor site wound had exudates and leg edema, whereas two other cases of SVG donor site wounds had slight redness around the wound, and another case had slight end-of-sternal wound dehiscence. In these four patients, the doctors concluded that the wounds were not infected but merely wound complications. The researcher consulted with the doctors and nurses in the team, which is considered a secondary prevention strategy, to detect early abnormal wounds. The researcher, as a nurse coordinator of the healthcare team and the patient or caregiver, provides timely treatment and reduces the severity of complications. The researcher provided health advice after consulting with the team’s physicians and nurses according to the symptoms and problems encountered after treatment to promote normal healing of the wounds, which is considered tertiary prevention. On the follow-up day, these four patients with wound problems had good wound healing, reduced redness, and leg edema.
In the control group, three patients were diagnosed with superficial incisional SSIs of SVG donor site wounds. They took antibiotics, and their wounds were cleaned. One patient was diagnosed with deep sternal wound infection, which was treated by reopening the sternal wound for cleaning and debridement, and antibiotics were then given. The patient visited the outpatient department every day to get the sternal wound cleaned.
For this study, most participants in both intervention and control groups had diabetes and obesity for more than ten years. In addition, the SVG donor site wounds of all the participants were conventional open techniques. Most of the lengths of SVG from the thigh to the ankle were longer than the length of the sternal wound. Therefore, the incidence of germs exposure in the SVG donor site wound may be higher than in the sternal wound. It is also possible that the healing process of the SVG donor site wound may be slower than the sternal wound. This may result in major SVG donor site wound complications, including lymphedema and redness around the wound, which increases the risk of SSIs (Tocharoenchok et al., 2017).
Although the blood glucose level was not an outcome for this study, at 14–21 days after the surgery, the blood glucose level in the intervention group decreased more than that of the control group. However, the difference was not significant. This may be due to the fact that the intervention group received knowledge and advice on glycemic control, making it possible to control blood glucose levels better and reduce the risk of delayed wound healing or the occurrence of infected wounds (Navaratnarajah et al., 2018).
Other confounding factors affecting wound healing, including hygienic wound care, frequency of dressing, types of dressing use, and dietary pattern, may have also been present, which we attempted to control and consider. Our study provided similar surgical wound care for the intervention and control groups. In the absence of fluid drainage from the wounds during hospitalization, the wounds were covered with gauze for 72 h. Cleaning of the wounds and changing dressings were performed for the first time on postoperative days 3–5 and the second time on postoperative days 6 and 7 or the date of hospital discharge. Generally, daily surgical wound cleaning is not required. In fact, nurses just need to ensure that the wound is kept clean and that the wound dressing does not get wet (Annesley, 2019). The wounds were covered with wound dressing until follow-up after discharge at 1–2 weeks. Gauze or film dressings were used to dress sternal and SVG donor site wounds for the intervention and control groups according to the physician’s discretion. Moreover, both groups had similar dietary patterns, with most patients beginning to develop an appetite and consuming more food after returning home.
Our study findings found that the intervention group had good sternal and SVG donor site wound healing. The TPWHP can help patients control their blood glucose, perform surgical wound care, and undertake various precautions, resulting in the SVG donor site having better wound healing than the control group; however, the results of this study did not show a clear difference in sternal wound healing. This may be due to the minimum number of samples analyzed, and the sternal wound healing of the two groups was mostly at a good level according to the wound healing process.
Furthermore, before the scheduled follow-up visit, the TPWHP could detect abnormalities or signs of infection early in the sternal and SVG donor site wounds. The researcher coordinates with the doctors and nurses in the team, enabling patients to receive timely treatment and reduce the severity of wound complications. Consistent with past studies, with telehealth interventions for monitoring surgical wound healing for two weeks after hospital discharge, abnormal or infection symptoms of the surgical wound can be detected early before the follow-up day (Ajibade et al., 2020; Gunter et al., 2018; Mousa et al., 2019; Sreedharan et al., 2022). The photos of the surgical wounds obtained using a smartphone can be used in monitoring the wound, surgical wound abnormalities, or SSIs after hospital discharge. These findings were confirmed by previous studies (McLean et al., 2021; Totty et al., 2018).
Implications of the Study for Nursing Practice
Nurses should implement the TPWHP for patients with diabetes undergoing CABG to facilitate more effective wound healing. It can help patients or caregivers acquire knowledge and understanding and appropriately implement wound healing promotion activities in addition to monitoring the wound and receiving additional advice on wound care after hospital discharge until the follow-up day. The TPWHP provides information on the role of cardiovascular nurses, which should be improved to provide quality care to patients undergoing cardiac surgery. In addition, the TPWHP can be used as a guideline for further studies.
Limitations of the Study
The timing of data collection for wound healing assessment on the follow-up day was not identical for all patients. Therefore, the researcher used a time period for assessing wound healing, i.e., days 14–21 after surgery. However, future studies should assess wound healing at the same time to reduce discrepancies in outcomes.
Conclusion
Even though wounds can heal naturally, proper wound care will more effectively facilitate the healing process. The TPWHP helps continuously monitor wound healing and care; as a result, the patients receiving the TPWHP with routine nursing care showed better SVG donor site wound healing than the patients receiving only routine nursing care. Moreover, it helps sternal wounds acquire good wound healing, although the difference was not significant. Therefore, nurses should implement the TPWHP in conjunction with a multidisciplinary team to facilitate more effective wound healing and achieve early detection of abnormal symptoms or signs of SSIs at the sternal wound and SVG donor site wound after hospital discharge.