Background
Peripheral intravenous cannulation (PIVC) is an invasive procedure in which a catheter is inserted through a patient’s skin into the lumen of a peripheral blood vein. This causes children severe pain and increases the anxiety of children and caregivers (Smith et al., 2007). It is a common stressful procedure for children, and nearly all pediatric patients have an experience with PIVC (Zingg & Pittet, 2009). This technique is mainly recommended for administering solutions, medications, blood, or blood products to pediatric patients (Doyle & McCutcheon, 2015).
If not managed quickly and decisively, the pain experienced by children can have long-term physical and psychological implications, such as needle phobia, avoidance of medical care, and a lack of cooperation during future medical procedures. Therefore, it is advisable to manage pain proactively during the insertion of the cannula or venous access (Kennedy et al., 2008). Reports show that relief of pain during painful procedures is an important responsibility of pediatricians, nursing staff, and other health personnel (Wong et al., 2012). The WHO affirms that pain relief is a fundamental human right (Daher, 2010). Therefore, it is significant to explore the most effective forms of pain management (Koller & Goldman, 2012; Uman et al., 2013).
The nurses are responsible for managing the pain and anxiety of patients as the most crucial results of painful procedures. It is the responsibility of pediatric nurses to anticipate, recognize, and evaluate pain and to implement interventions before, during, and after procedures. In order to treat pain effectively, Both pharmacologic and nonpharmacologic approaches have been strongly recommended in research studies and clinical guidelines (Czarnecki et al., 2011; Taddio et al., 2010).
A usual pharmacological strategy is the use of a topical cream to reduce pain resulting from medical procedures (Trottier et al., 2019). But children may experience pain and distress because of these creams (Gold et al., 2006). due to possible side effects. These creams have physiological effects with no impact on psychological perspectives, such as patients’ attitudes, while non-pharmacological methods help break the vicious cycle between pain and anxiety by controlling children’s pain and anxiety (Tick et al., 2018). Non-pharmacological methods are used because they are simple, easy to use, saves time, have no side effects, enhance interaction, and promote an individual sense of control over anxiety and pain (Short et al., 2017).
For these reasons, non-pharmacological approaches are generally recognized as alternative techniques, which may be used separately or in pair with pharmacological approaches to treat pain and anxiety and establish a sense of control over fear in children (Uman et al., 2013). Distraction techniques move children’s attention away from uncomfortable stimulation to more engaging or pleasant stimulation. They are easy-to-administer, inexpensive, and effective ways to decrease pain and anxiety levels (Koller & Goldman, 2012).
As a non-pharmacological technique, distraction is one of the most effective ways to reduce anxiety and pain. There are two kinds of distraction: active distraction and passive distraction (Aydin et al., 2016; Inan & Inal, 2019). Active distraction encourages children to take part in certain assignments during the procedure by stimulating one or more of their senses and engaging their skills during painful procedures. In contrast, with passive distraction, the children are not involved in activities during the therapeutic procedures. Passive distraction only activates their visual and/or auditory senses (Aydin et al., 2016; Inan & Inal, 2019). The benefits and effectiveness of distraction are documented through parent-child and/or observer reports on reducing pain, distress, and anxiety (Uman et al., 2013). Art therapy is a useful method of distraction. This method supports children in coping with stress before, during, and after medical procedures (Galvez et al., 2021; Woodgate et al., 2014).
Arts-based interventions have been reported to relieve pain and anxiety in children with a variety of different diseases and a variety of situations, such as children with cancer (Abdulah et al., 2019) and hospitalized children (Shella, 2018). The Trace Image and Coloring for Kids-Book (TICK-B) may be superior to other distraction interventions because many distraction techniques require training, are expensive, unattractive to children, complex to apply, and impractical, such as computer-related games, virtual reality, and electronic distraction. These factors hinder the widespread application of distraction methods in hospitals. In many clinical settings in developing countries, children do not receive any pharmacological or non-pharmacological interventions to decrease pain and anxiety levels. To date, to our knowledge, there are no studies on using the TICK-B as an art-based distraction to reduce children’s pain intensity and anxiety levels during PICV in the published research. The TICK-B technique is an art base-intervention easily applied by nurses. It does not require training or have adverse effects during medical procedures, and it is a cost-effective and attractive technique. For these reasons, in this study, we examined the effectiveness of the TICK-B in decreasing the pain and anxiety of hospitalized children during PICV. We hypothesized that children who received the TICK-B would have a significantly lower level of pain and anxiety.
Methods
Study Design
This was a parallel, randomized, double-blind clinical trial conducted on pediatric patients. Patients who required the PIVC procedure were randomly assigned into two groups: the intervention group and the control group.
Samples/Participants
The patients from the medical ward of the Heevi pediatric teaching hospital in the city of Duhok, Iraqi Kurdistan, were recruited between November 2019 and February 2020. The Heevi pediatric teaching hospital is the only pediatric hospital to treat medical, emergency, and surgical conditions in Duhok. The hospital has a CCU, NICU, operation unit, reception unit, and medical, emergency, and surgical wards.
The patients’ baseline information was assessed according to the eligibility criteria by the first author. In addition, the medical records of the patients were checked for the eligibility criteria. Accordingly, the eligible patients were randomly allocated to either the intervention or control group. The study sample included patients admitted to the pediatric medical ward aged 6–12 years old of both genders who required PIVC. We received consent from the children’s parents. Patients were excluded from the study based on having a chronic disease, being unconscious, being neuro-developmentally delayed (diagnosed through parental reporting), being unable to communicate verbally, having a hearing or sight impairment, or having taken an analgesic within the past 6 hours. The general characteristics of both groups of patients and their parents were similar.
We determined the sample size based on the G*power program (Faul et al., 2007). The pain level of the first five cases in the control group was assessed by the observer, and the mean value and standard deviation of these five cases were measured accordingly. The obtained score was 6.53 (SD = 1.5). We believed the intervention would have a large effect on pain in this study. Therefore, we assumed this value could decrease to 5.53 (SD = 0.85) after the intervention. The effect size was 0.820, two tails, α 0.05, and power (1-β), 0.95 was considered using the two independent groups. The required number of patients in each group was 40, but we increased our sample size by around 50% to avoid missing information due to possible technical issues. In addition, cases were widely available at the hospitals, and the intervention was easily conducted with a short follow-up time. Accordingly, these two factors allowed us to raise our sample size.
In the randomization process, the names of the patients who required the PIVC procedure were recorded on a pre-designed form. Simple randomization was conducted using an envelope technique. Opaque sealed envelopes containing information assigning patients to either the intervention or control group were given to the patients. The patients, nurses, and parents were blind to the groupings due to the opaque sealed envelopes. The observer nurse who measured pain and anxiety levels was unaware of the groups’ assignments. To reduce measurement bias, we did not allow the observer nurse to enter the room until the procedure ended. In addition, the nurse was masked as to whether the intervention was applied or not applied to a patient. We also coordinated with the head nurse of the medical ward so that no one would be allowed to enter the room and interrupt the procedure.
The patients were asked to select one of these envelopes. Of 110 invited patients, ten declined to take part in the study. The patients who agreed to participate in the study were randomly assigned into the groups. The intervention group included 48 patients, while the control group included 52 patients. To apply the allocation concealment, we selected one child randomly from each room for either inclusion in the experimental or control group. We asked the nurses to bring the patients to a special room for the study purpose (The intervention was not performed in the same room as the child admitted). The child selected an opaque pocket for either inclusion in the experimental or control group. This technique helped us avoid allocation bias since the patients did not know what had been done to other patients. Also, the rooms were separated from each other, and patients were not aware of the situation of the other children. In terms of information bias, the patients were not aware of the situation of other patients either in the ward or room.
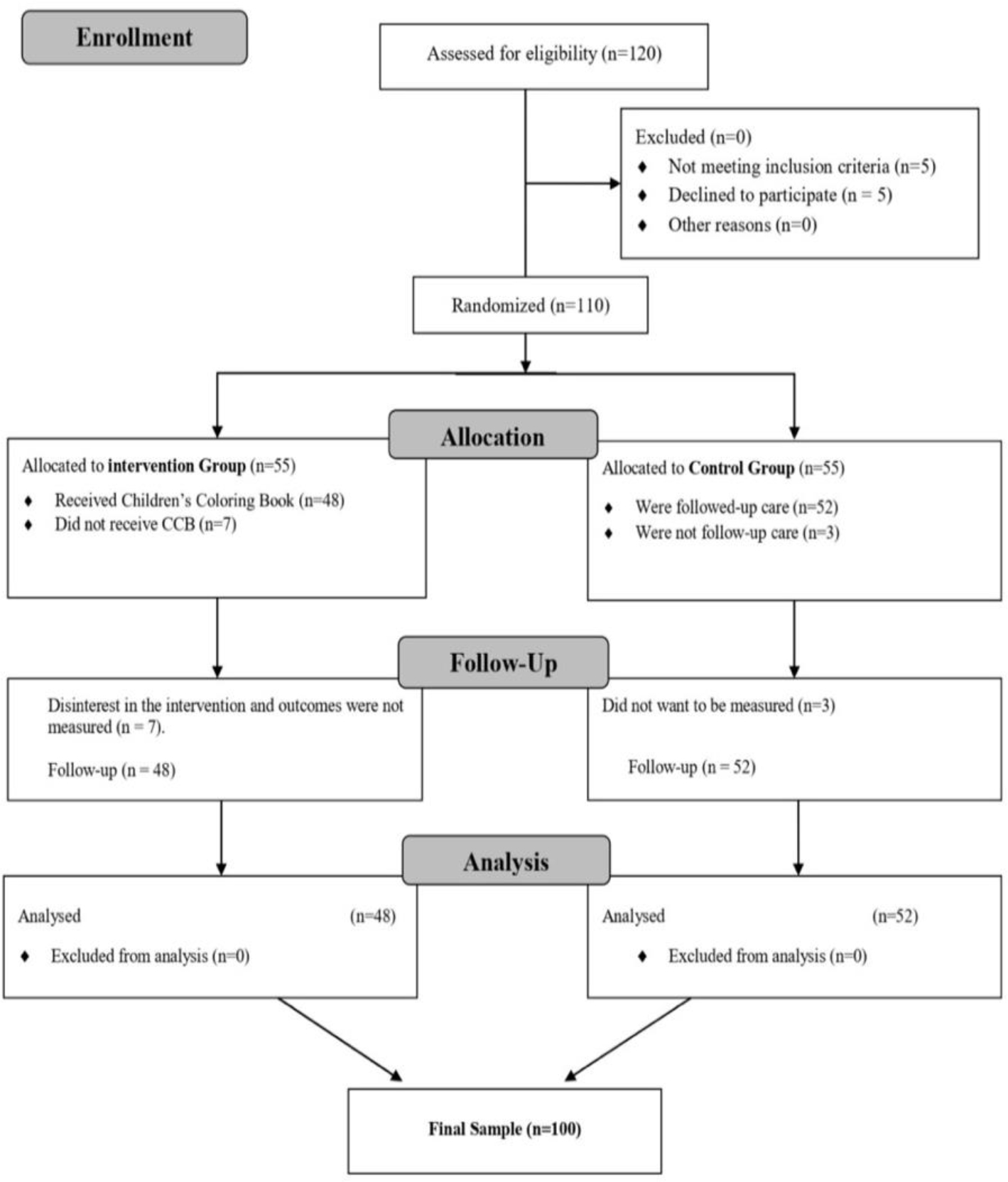
The children did not know that we were comparing their pain and anxiety levels with another group. We also asked the clinical nurse and parents not to inform their children about the intervention. Therefore, the children were completely blind to the goals of the intervention (see flow chart in Figure 1).
Intervention
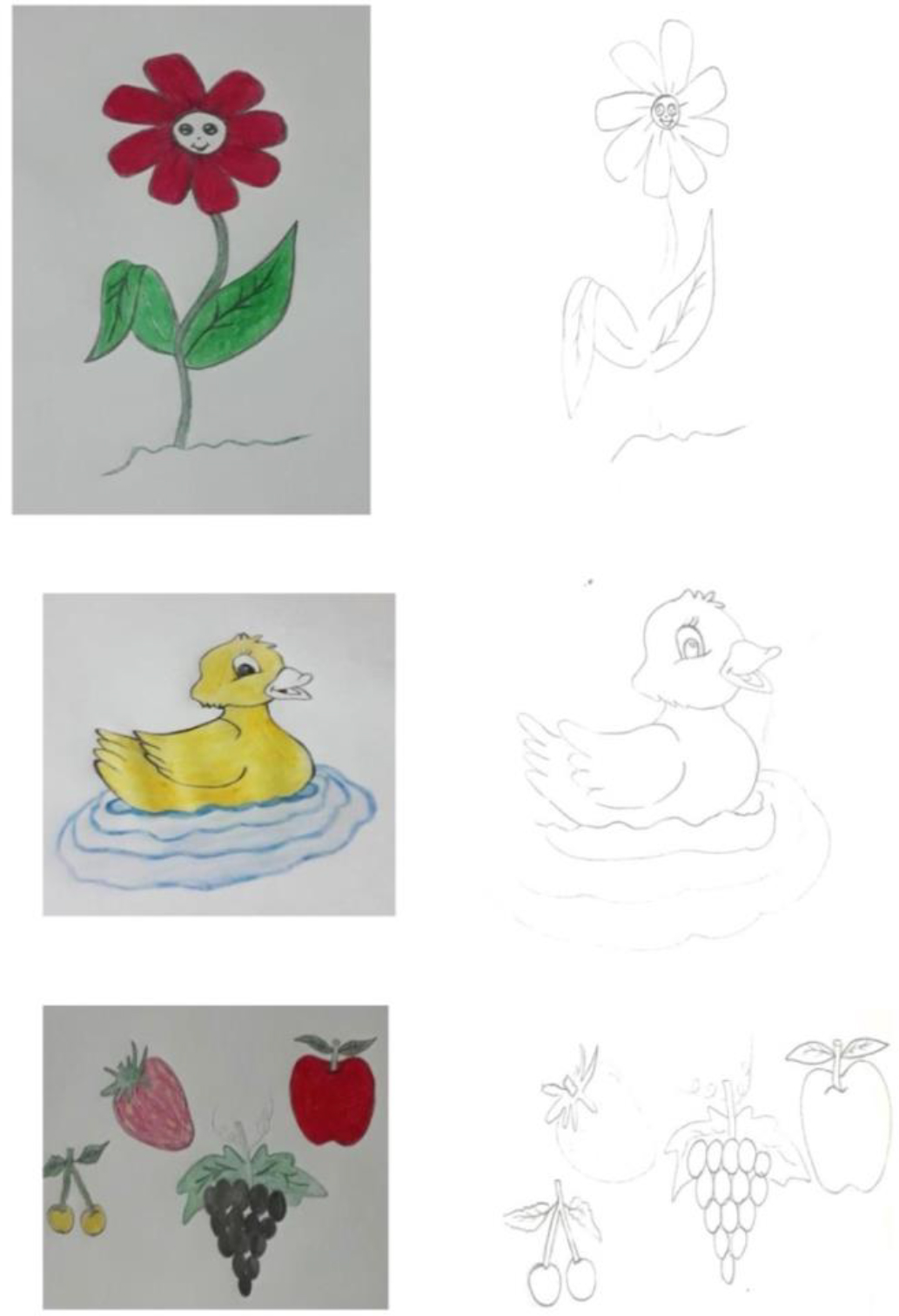
TICK-B was developed through the following two phases: Firstly, we consulted two child psychiatrists to obtain the types of images that must be included in the TICK-B tool. The psychiatrists gave us some hints about the effects of the images on the children’s behavior and mental status. They advised us that the image must be desirable and immersed with the nature perspectives and be free from the violent features. The pictures of the pets, such as rabbits and flowers, are considered convenient images.
In the second phase, we contacted the professional art teachers at three elementary schools for children in different geographic areas. We asked them to draw convenient images based on the advice of the psychiatrists. The teachers made several images at this phase. Then, the images were presented to the psychiatrists and the researchers to select the most appropriate pieces for inclusion in the TICK-B.
The first author initiated the TICK-B intervention between 2 and 3 minutes before the procedure and continued until the cannulation procedure was completed. The TICK-B was implemented by the first author, a Ph.D. student in pediatric nursing, but all of the outcome evaluations were conducted by the observer nurse, the parents, and the children. The observer nurse, who had experience in child health nursing for eight years, was trained by the researcher to assess pain and anxiety. The nurses made the decisions on the PIVC procedure in the pediatric wards on the same day. The clinical nurse who performed the PIVC procedure had over ten years of experience in child health care. For that reason, we did not educate the nurse about the PIVC procedure.
Peripheral vein cannulation was performed by the same nurse practitioner for all pediatric patients. The child was taken to a quiet place in the ward and sat at a table. Two to three minutes before beginning the procedure, the first author interacted with the child to gain the child’s confidence, cooperation, and friendship during the TICK-B intervention. Then, the book was handed over to the patient, instructed to choose a preferred image to be colored during the cannulation procedure. At this time, the first author started to apply the intervention simultaneously with the venipuncture procedure. Then, the clinical nurse started to perform the PIVC procedure. The observer nurse and the children’s parents were hidden for accurate study purposes to avoid behavioral changes during and after the procedure and to avoid measurement bias. Parents were allowed to remain with the children during the cannulation to standardize the cannulation procedure, and the cannula was placed on the left hand of each child. The method of pain relief (distraction) was continued until the procedure was completed. Our TICK-B technique was tested with ten children in a pilot study to assess TICK-B applicability. Examples of coloring images can be seen in Figure 2.
For the control group, the patients received routine hospital care during cannulation procedures. They did not receive a TICK-B intervention or any other kind of distractions as non-pharmacological or pharmacological approaches. In addition, the child’s mother was allowed to be presented during the cannulation procedure as recommended by clinical guidelines.
Data Collection
The children were asked to report outcomes after the 1–2-minute-long procedure ended. The children rated their pain and anxiety levels based on the Faces Pain Scale-Revised (FPS-R) and Children’s Fear Scale (CFS). The observer nurse and parents used the visual analog scale (VAS) to measure anxiety levels and pain intensity in children. We were permitted to use these tools, and they were very easy to use since they were pictures and did not require translation into another language. The pain and anxiety levels were separately evaluated by assessors, including children, parents, and the observer nurse. The assessors were masked from each other in this study to avoid possible measurement bias. The observer nurse had no personal conflicts or financial interest in the study.
Instruments
The general features of the patients—including age, gender, hospitalization, frequency of injections, parents’ age, and educational status—were recorded using a pre-designed questionnaire.
Pain in children (self-assessment): Faces Pain Scale-Revised (FPS-R) was used to measure pain severity. The FPS-R ranges from 0 to 10 and illustrates degrees of pain with six cartoon expressions ranging from “no pain” to “very painful.” The children were encouraged to select the face that was compatible with their pain severity. The FPS-R scale is unique and has been proven to be reliable in assessing pain in children (Thong et al., 2018).
Anxiety in children (self-assessment): To measure anxiety in children, the Children’s Fear Scale (CFS) was used. This tool was applied to measure the fear of children aged 5 to 10 years during painful procedures. It includes illustrations of 5 faces placed equally on a horizontal plane. The CFS faces each express a different level of anxiety. On the far left of the scale, there is a face marked with the number 0, representing an expression of no anxiety at all, and on the far right, there is a face marked with the number 4, marked with the greatest level of anxiety. The CFS is a viable and reliable instrument for measuring procedural anxiety in school-aged children (McMurtry et al., 2011).
Anxiety and pain (proxy assessment): The observer nurse and parents assessed the children’s state of pain and anxiety using a Visual Analog Scale (VAS). When the VAS score is 0, no pain is felt, and when it is 10, the most severe discomfort is experienced. After the cannulation was completed, the observer nurse and parents reported their assessment of the levels of anxiety and pain on scales from “no anxiety” to “greatest anxiety” and “no pain” to “worst pain.” The VAS is a valid and reliable scale. Therefore, it is commonly used for measuring outcomes of painful procedures in children 8–18 years of age (Bailey et al., 2012).
Data Analysis
The general features of all pediatric patients in the study were demonstrated in mean (Sta. deviation) or no (%). Independent t-tests or Pearson Chi-Square tests were performed to assess the homogeneity of patients in both groups. A comparison of pain and anxiety levels between the intervention and control study groups was conducted using an independent t-test in “per-protocol” analysis. We didn’t have measurements for the few cases that were lost to follow up in the study. Comparisons of pain and anxiety over time between the study groups were conducted with a paired t-test. The anxiety and pain levels were compared between the intervention and control groups using an independent t-test. Also, the correlation between fear and pain and the role of children’s characteristics and previous pain on later fear was investigated using bivariate correlation and linear regression. We didn’t have measurements for the outcomes of the few cases that were lost to follow-up in the study. A p-value of less than 0.05 was deemed a significant level of difference. For the statistical analysis, IBM SPSS Statistics for Windows was used (Version 25.0; Armonk, NY, 2017).
Ethical Considerations
This paper was part of a PhD program. Ethical approval was given by the Division of Scientific Research, Directorate of Planning, Duhok General Directorate of Health in Duhok on September 10, 2019 (registration number 10092019-6). The grant to publish the results of this study was obtained on August 23, 2020 (reference number 20072020-3). Administrative approval was also received from Heevi Hospital. According to the terms of the Declaration of Helsinki, informed written consent was gained from the parents of all children before enrollment in the study. We did not perform any harmful intervention on the patients in this study.
Results
The authors considered 120 children for inclusion in this study, 110 of whom were eligible and participated; ten were not included because they were too young. Of the 110 included in this study, the parents of ten of them declined the procedure: seven patients in the intervention group and three in the control group. The patients in both study groups were similar in age, gender, number of injections, maternal age, and education (Table 1).
| Patients’ characteristics | Study groups | Statistic value (Chi Square/t/Fisher) | p-value (two-sided) | |
|---|---|---|---|---|
| Control (n = 52) | Intervention (n = 48) | |||
| Age (year); Mean (SD) | 7.98 (1.96) | 7.79 (1.78) | 0.998 | 0.321a |
| Hospitalization day; Mean (SD) | 3.38 (1.05) | 3.33 (1.04) | 0.245 | 0.807a |
| Number of injection attempt; Mean (SD) | 1.13 (0.34) | 1.23 (0.42) | -0.954 | 0.342a |
| Mother age (year); Mean (SD) | 40.98 (3.97) | 40.46 (4.31) | 0.631 | 0.530a |
| Gender; no (%) | ||||
| Male | 25 (48.1) | 24 (50.0) | 0.037 | 0.848b |
| Female | 27 (51.9) | 24 (50.0) | ||
| Mother’s education; no (%) | ||||
| Illiterate | 4 (7.7) | 4 (8.3) | 1.175 | 0.907c |
| Primary school grad. | 25 (48.1) | 19 (39.6) | ||
| Secondary school grad. | 14 (26.9) | 16 (33.3) | ||
| High school grad. | 4 (7.7) | 5 (10.4) | ||
| College grad. | 5 (9.6) | 4 (8.3) | ||
The patients in the intervention group reported a significantly lower level of pain during the procedure (t = 11.37; p < 0.001) with a medium effect size (2.27) and after the procedure (t = 12.08; p < 0.001) with a medium effect size (2.43) compared to the patients in the control group. The same pattern was observed for anxiety during the procedure (t = 16.76; p < 0.001) with a medium effect size (3.34) and after the procedure (t = 17.00; p < 0.001) with a medium effect size (3.41). The patients in the intervention and control groups had similar anxiety and pain levels before starting the cannulation procedure (p > 0.05). The study did not find statistically significant differences in pain and anxiety over time in the control group, while pain and anxiety levels decreased significantly over time in the intervention group (Table 2).
| Pain and anxiety | Study groups | t | Degree of freedom (df) | p-value (two-sided) | Effect size (Cohen’s d) | |
|---|---|---|---|---|---|---|
| Control (n = 52) | Intervention (n = 48) | |||||
| Previous pain | 7.13 (1.78) | 7.00 (1.75) | 0.381 | 98 | 0.704 | NA |
| Pain during procedure | 7.12 (1.75) | 3.27 (1.64) | 11.37 | 98 | <0.001 | 2.27 |
| Pain after procedure | 7.06 (1.68) | 3.08 (1.59) | 12.08 | 98 | <0.001 | 2.43 |
| Anxiety pre procedure | 3.25 (0.59) | 3.19 (0.60) | 0.522 | 98 | 0.603 | NA |
| Anxiety during procedure | 3.19 (0.59) | 1.13 (0.64) | 16.76 | 98 | <0.001 | 3.34 |
| Anxiety after procedure | 3.17 (0.64) | 0.88 (0.70) | 17.00 | 98 | <0.001 | 3.41 |
a an independent t-test was performed for statistical analyses
Pain and anxiety levels were measured by WBFS, VAS, and CFS, respectively
Pain and anxiety scores were significantly lower in the intervention group compared to the control group as evaluated by children, parents, and the observer nurse (Table 3). Pre-procedure pain and other medical conditions did not contribute to post-procedure anxiety (Table 4).
| Outcome measurements | Study Groups Mean (SD) | t | Degree of freedom (df) | Effect size (Cohen’s d) | |
|---|---|---|---|---|---|
| Control group (n = 52) | Intervention group (n = 48) | ||||
| Pain | |||||
| Child reported | 7.06 (1.68) | 3.08 (1.59) | 12.08 | 98 | 2.43 |
| Parent reported | 7.13 (1.70) | 3.08 (1.56) | 12.34 | 98 | 2.48 |
| Observer reported | 7.13 (1.69) | 3.06 (1.60) | 12.33 | 98 | 2.47 |
| Fear | |||||
| Child reported | 3.17 (0.64) | 0.88 (0.70) | 17.00 | 98 | 3.41 |
| Parent reported | 3.19 (0.84) | 0.94 (0.72) | 14.29 | 98 | 2.87 |
| Observer reported | 2.94 (0.80) | 0.85 (0.68) | 13.95 | 98 | 2.81 |
The p-value of the pain and anxiety was p < 0.001 for all comparisons
Pain and anxiety were measured by WBFS, VAS, and CFS, respectively
| Controlling factors | Dependent variable: Anxiety after the procedure | ||||
|---|---|---|---|---|---|
| Standardized Coefficients Beta | t | p-value | 95% CI for B | ||
| Lower Bound | Upper Bound | ||||
| Previous pain | -0.269 | -0.759 | 0.452 | -0.397 | 0.180 |
| Previous anxiety | -0.257 | -1.683 | 0.100 | -0.655 | 0.060 |
| Age | -0.321 | -0.876 | 0.386 | -0.416 | 0.165 |
| Gender | -0.018 | -0.115 | 0.909 | -0.475 | 0.423 |
| Hospitalization days | -0.181 | -1.019 | 0.315 | -0.367 | 0.121 |
| Attempt | 0.007 | 0.045 | 0.964 | -0.502 | 0.525 |
| Mother age | 0.059 | 0.364 | 0.718 | -0.044 | 0.064 |
| Mother education | -0.147 | -0.880 | 0.384 | -0.324 | 0.128 |
The linear regression was performed for statistical analyses
Discussion
This study demonstrated that distraction using the TICK-B is effective in lowering pain and anxiety levels in hospitalized children reported either by the children themselves, parents, or observer nurse. This study used the TICK-B technique for the first time as an art-based distraction in school-aged children. Pain is often felt during procedures routinely conducted in hospitals, such as phlebotomies and peripheral intravenous cannulation. In children, pain may cause tension, fear, and anxiety (Gold et al., 2006). The American Pain Society recommends providing effective pain management both before and during needle procedures (Czarnecki et al., 2011). According to evidence-based clinical practice recommendations, most situations involving pain and anxiety induced by painful procedures can be managed with non-pharmacological approaches (Bergomi et al., 2018). According to our hypothesis, art intervention based on the TICK-B could reduce the levels of pain and anxiety in school-aged children.
Consistent with our study, a nonrandomized controlled trial showed that children who received art therapy exhibited cooperative behavior and desired art therapy intervention for future painful procedures. In comparison, the children in the control group who did not receive art intervention showed resistance, uncooperative behavior, and fear during and after lumbar insertion and marrow aspiration (Shella, 2018). The literature has confirmed the effectiveness of art-based interventions in relieving pain and anxiety among children with various diseases.
Children’s fear of medical procedures decreases when they actively participate in a task during therapeutic interventions. It seems that the active participation of the children increases their tolerance toward the pain posed by medical interventions (Aydin et al., 2016; Inan & Inal, 2019). The reason for this increased tolerance may be an altered perception of pain in the children.
The pain relief experienced during therapeutic procedures when children actively participate in a task may be explained by the following theories. Melzack and Wall’s gate-control theory of pain, suggested in 1965, may explain how art-based intervention affects the perception and experience of pain and anxiety during therapeutic and diagnostic procedures. In the gate-control theory, the brain has a neural gate mechanism that releases or suppresses an individual’s perception of pain. In addition to past events and emotions, psychological factors, such as awareness, also influence pain perception. The gates open due to stress or when there is a lack of activity and only a painful stimulus to focus. An individual, therefore, perceives a higher degree of pain when the gates are open. The gates close when the feeling of pain is reduced by relaxing the person, diminishing the painful activity, or using a distracting stimulant (Melzack & Wall, 1965).
There are different logical interpretations of the distraction’s function. One of the earliest scientific principles for treating pain transmission is the gate control theory. According to the theory, the central nervous system modifies the experience of pain, and so cognitive attention can influence pain processing and perception (Melzack & Wall, 1965). This effect may be analyzed neuro-psychologically, as certain areas of the brain are less active during distracting tasks (Seminowicz & Davis, 2006).
A second explanation, one in harmony with gate-control theory, can be found in limited attentional capacity theory, which proposes that the resources available to process pain are fewer if some attention is devoted to a distracting job (Gutiérrez-Maldonado et al., 2012). Attention plays an essential role in the perception of children’s pain during painful procedures. In this regard, the children’s pain increases when there is no distraction task during the therapeutic procedures. We believe that TICK-B has played a distraction role in reducing the children’s attention to the painful procedures.
A third explanation is offered by the behavioral concept a distraction introduces a stimulus with prior positive associations (e.g., a favorite game), stimulating behaviors that do not correspond to the behaviors of someone in pain (e.g., smiling in a film), and strengthening painless reactions (Pancekauskaite & Jankauskaite, 2018). The most common pain management strategy used on children is controlling their attention by engaging in pain-distracting conversations or activities. We hypothesize that distraction involves a competition for attention between sensory pain and another activity. In accordance with the literature, the TICK-B reduces pain by providing distracting tasks for children.
Distractions may decrease the stress caused by therapeutic procedures in children and enable children to be more tolerant of pain. In this regard, children may become more relaxed, satisfied, and active and allowing nurses to concentrate on delivering high-quality care better. In addition, during distraction tasks, children’s domain raises awareness of the self and others. This awareness assists children in coping with stress and traumatic experiences (Dalley & McMurtry, 2016).
Effective coping is associated with managing a situation’s demands or controlling emotions by gaining a sense of physical and psychological well-being (Folkman & Lazarus, 1984). In pediatric psycho-oncology, One of the most crucial research areas was how to help children deal with therapies, particularly invasive medical procedures (Askins & Moore, 2008).
Gloria Martinez-Ayala, a psychologist, claims that art-based intervention activates several regions of the brain. The potential effects of art therapy include the diminishment of symptoms associated with stress, minimization of anxiety and depressive moods, conflict resolution, increased quality of life, and visual thinking (Caddy et al., 2012). In addition, the associated relaxation and mindfulness modulation lower the activity of the amygdala is a key component of the brain involved in managing emotions affected by stress (Taren et al., 2015). We believe that the reduction in pain and anxiety experienced during art-therapy intervention is due to this kind of activation in the brain.
The strengths of this study include the performance of randomization, the recruitment of a control group, the use of simple pain and fear assessment tools, practical art-based intervention, blinding, and allocation concealment. However, the study was not free from limitations. To reduce the reporting bias of the parents, the outcomes were also reported by two other assessors. In addition, we included school-age children in this study, limiting the applicability of the TICK-B to this age group. Furthermore, we recruited patients from a single site and a singles ward.
Implications for Nursing Practice
An essential role of pediatric nurses during painful interventions is to improve nurse-child collaboration by reducing the emotional and physical impact of medical interventions through non-pharmacologic approaches. As an art-based distraction, the TICK-B is a non-pharmacologic technique and an enjoyable activity that helps distract children and decrease levels of pain and anxiety during cannulation. Nurses can use the TICK-B as a simple, cost-effective, and convenient technique to manage pain and anxiety in children.
Conclusion
The TICK-B art-based distraction technique was found to be an effective method in reducing the anxiety and pain of children during and after a cannulation procedure. In addition, the distraction technique can be used safely and does not adversely affect the success of the cannulation procedure. More research could be carried out to investigate whether the TICK-B is effective in diverse clinical settings across various age groups and cultures.