Background
The global concern regarding exposure to harmful substances in the air, water, and land is increasing. Emerging harmful substances contaminate various aspects such as food, water, personal care products, ambient air, vegetation, and agriculture (Yadav et al., 2021). Low and middle-income countries are particularly affected, and it is projected that by 2050, nearly 50% of the global population will reside in urban areas, leading to issues like overcrowding, poor air quality, and the spread of airborne infections (Reis et al., 2021). In Thailand, the measured annual mean PM2.5 in 2021 varied between provinces, ranging from 12.7 to 31.7 μg/m3, with an overall mean exposure of 21.3 μg/m3, which is four times higher than the standards set by the World Health Organization (Farrow et al., 2022). These findings highlight the abundance of harmful substances in the environment, posing a significant risk of exposure to all populations, including pregnant women.
Pregnancy is a period of increased vulnerability to the harmful substances present in the environment (Boyles et al., 2021). Disturbingly, a significant proportion of Thai pregnant women, approximately 42.50%, were found to have unacceptably high levels of lead in their bodies (Waeyeng et al., 2022). Furthermore, organophosphate was detected in 98% of infants’ meconium samples from mothers residing in agricultural areas (Onchoi et al., 2020). Prenatal exposure to these harmful substances has been linked to teratogenic effects, resulting in various birth defects or congenital anomalies affecting the structure and function of the developing fetus. Examples of these include congenital heart defects (Sun et al., 2023), cleft lips/palate (Lacerda et al., 2021), and developmental retardation (Bjørklund et al., 2019). The impact of harmful substances on the fetus depends on their specific characteristics, the amount and frequency of exposure, the placental mechanism, and the stage of fetal development (Cunningham et al., 2022).
Globally, birth defects contribute to an estimated 240,000 neonatal deaths within the first 28 days of life each year and an additional 170,000 deaths among children aged one month to five years (World Health Organization, 2022). These birth defects also result in significant financial burdens, with hospitalizations related to birth defects costing as much as $22.2 billion in the United States, accounting for 4.1% of all hospitalization costs and 7.7% of inpatient medical expenses (Swanson, 2023). It is worth noting that approximately 94% of severe birth defects occur in low- and middle-income countries (World Health Organization, 2022). In Thailand, out of the 175,370,320 surveyed children in 2021, there were 214,010 reported cases of birth defects (National Statistical Office, 2023). Additionally, 25% of Thai children experienced delayed development (National Institute of Child Development, 2020). Caregivers within families perceived the task of caring for children with birth defects as challenging, requiring significant physical and psychological efforts, leading to increased stress, decreased self-esteem, and financial and employment difficulties (Ahiable, 2020). Given these serious consequences, it is crucial to prioritize the prevention of exposure to harmful substances during pregnancy.
The practices of pregnant women play a crucial role in protecting against prenatal exposure to harmful substances. Pregnant women take various precautions to avoid exposure to harmful household products, such as refraining from using hair dyes, insecticide sprays, mosquito repellents, and home paints (Teysseire et al., 2019). They also avoid self-medication (Sychareun et al., 2022) and limit seafood consumption due to concerns about mercury contamination (Schaefer et al., 2019). However, despite these efforts, daily practices can still result in harmful exposures, such as environmental tobacco smoke (Oktalia, 2023) and exposure to cleaning chemicals in occupational settings (Herrin et al., 2023). In Thailand, for example, pregnant women continue to work in industrial factories where they face risks of exposure to harmful chemicals (Nuampa et al., 2020). Additionally, a study conducted in southern Thailand revealed that 54.49% of pregnant women had incorrect practices of washing fruits and vegetables by soaking them in non-running water, and only 45.51% had moderate knowledge about safe consumption behaviors regarding pesticide residues on fruits and vegetables (Thammarat et al., 2020).
Although there is a plethora of literature on the practices of pregnant women regarding harmful substances, most of the previous studies have been conducted in Western countries. It is essential to consider the cultural disparities between the East and the West, as the results may not be universally applicable to the Asian context. Furthermore, there is a lack of qualitative exploration that provides in-depth insights into the perceptions and experiences of pregnant women regarding this phenomenon. Therefore, our study aimed to explore the experiences of pregnant women in avoiding harmful substances in their daily lives to protect their unborn babies.
This issue is relevant for nursing because nurses play a vital role in supporting and promoting the health and well-being of pregnant women and their unborn babies. As frontline healthcare professionals, nurses are in a unique position to educate and empower pregnant women about the potential risks associated with exposure to harmful substances during pregnancy. By understanding the experiences, perceptions, and practices of pregnant women regarding harmful substances, nurses could ultimately contribute to improved maternal and fetal outcomes.
Methods
Study Design
This study employed a qualitative descriptive approach to fulfill its research aim. The qualitative descriptive method aims to provide a comprehensive summary of specific events experienced by individuals using everyday terms (Lambert & Lambert, 2012). The data collection process was based on a naturalistic inquiry method, which sought to elicit and capture individuals’ unique experiences and perspectives related to their practices (Sandelowski, 2000). The study using this approach acknowledged the inherent value and significance of the individual, emphasizing that their experiences cannot be disregarded but should be considered in constructing their reality. To enhance the practical applicability of the findings among practitioners, the research focused on non-interpretive inquiry and presented the results in a language that reflects everyday life rather than relying on conceptual, philosophical, and abstract terms (Sandelowski, 2000).
Participants
The participants were purposively selected based on specific inclusion criteria, including being Thai, aged between 18 and 35 years, and having a gestational age ranging from 12 to 34 weeks without high risks. Initially, nurses working in the clinics identified potential participants by reviewing the maternal and child health records. Subsequently, the researcher approached these individuals in person to ensure they met the inclusion criteria. The eligible women were provided with a clear explanation of the research. Data saturation, the point at which no new information or themes emerge from the interviews, was achieved after conducting interviews with 17 participants (Lincoln & Guba, 1985).
Data Collection
Data were collected in two hospitals located in urban and rural areas of Nakhon Si Thammarat Province in southern Thailand. The Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines (Tong et al., 2007) were followed to ensure transparency and adherence to reporting standards. The data were collected from September 2020 to April 2021. Prior to the study, there was no existing relationship between the researcher and the participants. Therefore, rapport was established gradually throughout the study, beginning from the initial contact until the completion of each interview.
The interviews were conducted by the first author, a female PhD candidate, in private and convenient settings such as the participant’s home or counseling room in the antenatal clinic. Each interview consisted of 2-3 sessions, ranging from 40 to 60 minutes. A semi-structured interview guide was utilized, with open-ended questions to explore the participants’ understanding of harmful substances to their unborn babies and their daily practices to prevent or avoid exposure. The interview guide included questions such as “From your understanding, what substances are harmful to your unborn baby?” and “In daily life, what do you do to avoid or prevent your unborn baby from harmful substances? Why and How?” Probing techniques were employed by the researcher to delve deeper into important issues and obtain comprehensive data, ensuring a thorough interpretation of the participants’ experiences. Throughout the interviews, the researcher sought permission to audio record the sessions to provide accurate capturing of the data.
Data Analysis
Data collection and analysis occurred concurrently in this study. Once data saturation was achieved, the in-depth interviews were transcribed verbatim in Thai. Manual thematic analysis (Sandelowski, 2000) was employed to analyze the data. The researcher followed the following steps: 1) repeated listening to the participants’ voices; 2) verbatim transcription of the interviews; 3) extensive reading and re-reading of the transcriptions to gain a comprehensive understanding of the entire data set; 4) coding the data to generate descriptive labels; 5) grouping codes into sub-themes; 6) identifying commonalities and patterns among sub-themes to form overarching themes; and 7) reviewing and refining sub-themes and themes in alignment with the research questions and existing literature. Finally, the findings were translated from Thai to English for reporting purposes.
Trustworthiness/Rigor
Trustworthiness was ensured through credibility, transferability, dependability, and confirmability (Lincoln & Guba, 1985). Credibility was established by conducting member checking with three participants, who were given the opportunity to review the tentative themes derived from the data analysis. Importantly, none of these participants provided contradictory opinions about the tentative results. Peer debriefing was held twice with qualitative research experts to verify the data collection and analysis processes. Detailed information about the participants and the study context was provided to enhance transferability. Dependability was achieved by conducting pilot interviews with two pregnant women who shared similar characteristics with the study participants. Additionally, discussions with the advisory committee were held to ensure consistency and accuracy in data analysis, findings, and interpretation. Confirmability was maintained by maintaining a reflexive journal and field notes throughout the study. These documents were regularly written before and after each interview, as well as during the data analysis process. This practice helped to prevent bias and ensure the accurate interpretation of the data.
Ethical Considerations
The research was approved by the Research Ethics Committee of the Faculty of Nursing, Chiang Mai University (Study Code: 2019-FULL026. Prior to participation, eligible women were provided with a detailed explanation of the research objectives, procedures, confidentiality measures, potential risks and benefits, their contribution to the study, and their rights to refuse or withdraw from participation. Written consent was obtained from all participants. Code numbers were used instead of personal identifiers throughout the study to protect anonymity. After completing the interviews, all participants received printed materials containing information about harmful substances. The researcher addressed any concerns or questions raised by the participants. As a token of appreciation for their time and contribution, participants received compensation of 100 THB (equivalent to 2.80 USD) for each interview. When the interviews coincided with the participants’ working hours, they were provided appropriate compensation to ensure fair remuneration.
Results
All 17 participants remained engaged until its completion. The participants’ ages ranged from 19 to 34 years old. The majority identified as Buddhists and had an educational background below a bachelor’s degree. Among the participants, three were health personnel, and six were employed in occupations involving exposure to chemical substances, such as beauticians, cleaning staff, factory workers, and farmers.
Additionally, eight participants had occupations with low exposure to harmful substances, including housewives, clerical/procurement officers, accountants, teachers, and bakers. The average monthly family income ranged from 6,000 THB (182.26 USD) to 50,000 THB (1,518.83 USD). Most of the participants were multiparous, while six were primiparous. None of the participants had attended health education classes specifically focused on harmful substances and birth defects (Table 1).
| ID | Age | Religion | Education | Occupation | Family Income THB (USD) | Living Area | Gravida | Health Education |
|---|---|---|---|---|---|---|---|---|
| 1 | 27 | Buddhist | Bachelor’s degree | Fruit farmers | 10,000 (303.77) | Rural | 2 | No |
| 2 | 34 | Buddhist | Master’s degree | Nurse | 25,000 (759.42) | Urban | 2 | No |
| 3 | 33 | Buddhist | Master’s degree | Pharmacist | 50,000 (1,518.83) | Urban | 2 | No |
| 4 | 30 | Christian | Bachelor’s degree | Teacher | 35,000 (1,063.18) | Urban | 2 | No |
| 5 | 25 | Buddhist | Upper secondary | Baker | 15,000 (455.65) | Sub-urban | 1 | No |
| 6 | 25 | Buddhist | Primary | Cleaning staff | 9,000 (273.39) | Rural | 3 | No |
| 7 | 28 | Buddhist | Upper secondary | Gold leaf factory worker | 20,000 (607.53) | Rural | 1 | No |
| 8 | 32 | Buddhist | Bachelor’s degree | Nurse | 40,000 (1,215.07) | Urban | 1 | No |
| 9 | 28 | Buddhist | Bachelor’s degree | Clerical/procurement officer | 30,000 (911.30) | Urban | 1 | No |
| 10 | 19 | Buddhist | Primary | Fruit farmer | 6,000 (182.26) | Rural | 2 | No |
| 11 | 30 | Buddhist | Upper secondary | Fruit juice vendor | 10,000 (303.77) | Urban | 3 | No |
| 12 | 31 | Muslim | Bachelor’s degree | Accountant | 18,000 (546.78) | Urban | 1 | No |
| 13 | 27 | Buddhist | Primary | Fruit farmer | 6,000 (182.26) | Rural | 3 | No |
| 14 | 30 | Buddhist | Lower Secondary | Beautician | 15,000 (455.65) | Rural | 4 | No |
| 15 | 22 | Buddhist | Diploma | Housewife | 6,000 (182.26) | Rural | 1 | No |
| 16 | 31 | Buddhist | Bachelor’s degree | Clerical/procurement officer | 30,000 (911.30) | Urban | 3 | No |
| 17 | 28 | Buddhist | Diploma | Accountant | 30,000 (911.30) | Sub-urban | 2 | No |
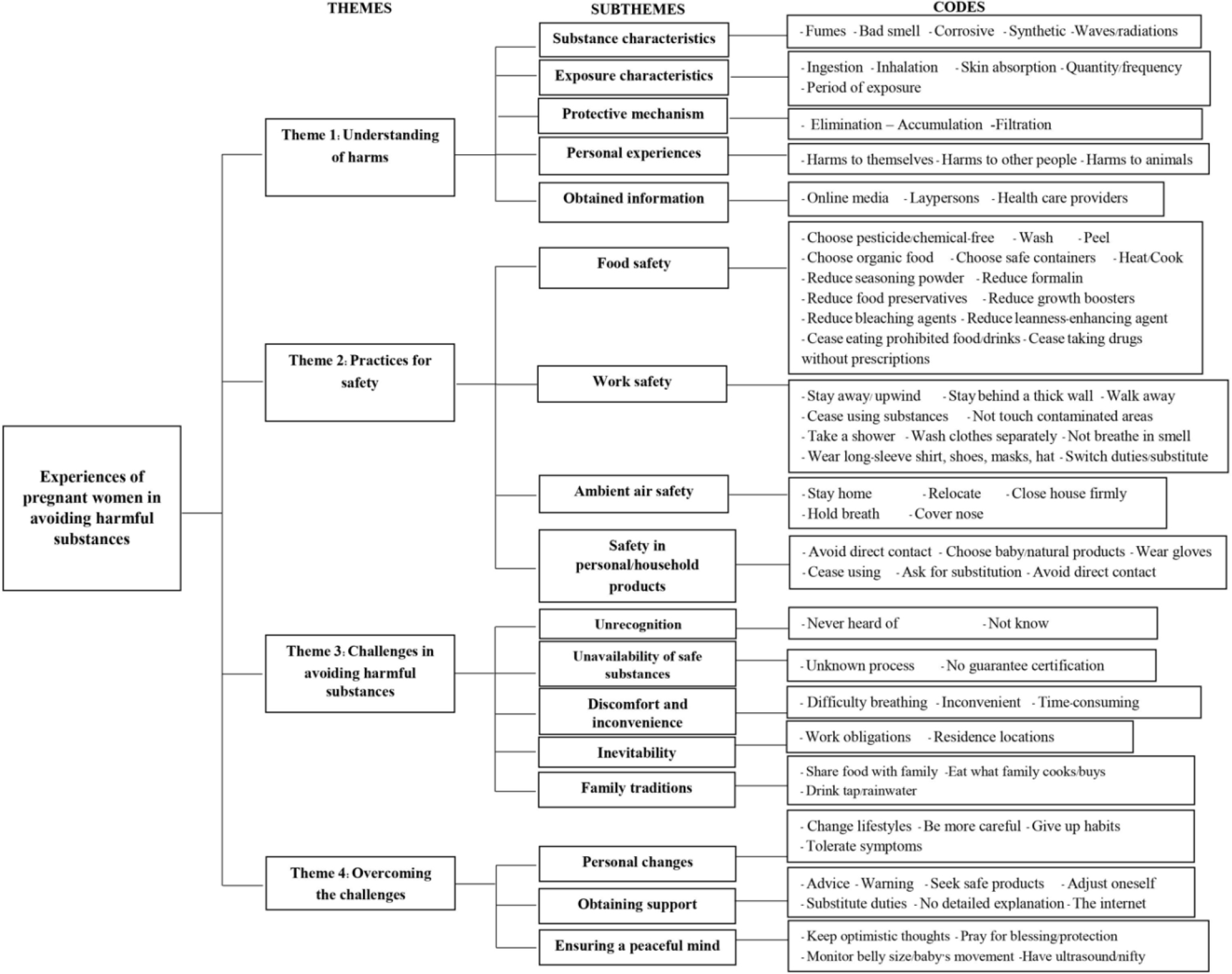
The participants’ experiences in avoiding harmful substances to their unborn babies emerged into four themes with 17 subthemes, as presented in Figure 1.
Theme 1: Understanding of Harms
When deciding if the substances were harmful or not, the participants based their understanding on the characteristics of substances and exposure and the body’s protective mechanism. In addition, they incorporated their personal experiences and obtained information.
Substance characteristics
Participants perceived that harmful substances tended to have harmful characteristics (e.g., fumes, bad and strong smell, and corrosive properties), synthetic compositions, and waves or radiations.
“Bathroom-cleaning products may be harmful to the baby because they’re corrosive. When using them to clean bathrooms, stains on the walls and floors come off, and we can see bubbles from corrosion.” (Participant 16)
“Paracetamol might affect unborn baby because medicines are synthesized chemical substances.” (Participant 9)
“I fear that having too much ultrasound will affect my baby…the radiations, the waves.” (Participant 3)
Exposure characteristics
Participants based their understanding on how the harmful substance was exposed. They believed exposure through ingestion and inhalation were harmful than skin absorption. Application of external-use products in the area distant from the belly might not endanger the unborn baby. The greater quantity and frequency of exposure would bring more harm. The most vulnerable period for harmful substance exposure was believed to be the early phase of pregnancy because it was the period of organ forming, and the unborn baby was vulnerable.
“Through the skin, it may not penetrate that deeply and may not reach the baby. But there may be higher chance through inhalation.” (Participant 12)
“For floor-mopping products, if the amount is small, it may be OK because I don’t touch it directly. But if the amount is large, it’s not OK and may affect the baby, causing the baby to get insufficient oxygen transmission through the umbilical cord.” (Participant 8)
“Toxic fumes such as exhaust fumes may be harmful, especially in the early pregnancy period like before four months of pregnancy when the baby’s organs are forming.” (Participant 2)
Body’s protective mechanism
Participants revealed that mechanisms related to the body played a role in how harmful substances affected the baby through the elimination and accumulation of substances, as well as filtration of harmful substances.
“For hair dye, I don’t think there’ll be any residues because the 2-month interval’s a long time. The residues should be eliminated through the stool.” (Participant 15)
“The placenta has a defense mechanism that can filter the harmful substances to some extent.” (Participant 2)
“Harmful substances may not reach the inner tissue where the baby is. The baby is in the amniotic sac that can protect the baby.” (Participant 17)
Personal experiences
Participants drew their understanding of harmful substances from their past personal experiences of observing harm to themselves, other people, and animals.
“I think lipstick’s harmful based on my personal experience. Before using this lipstick, my lips were not dark, but they got darker and darker after I used it.” (Participant 9)
“I used skincare cream and taken weight loss pills for over a year. There might be some residues, so I stopped before I got pregnant. When I was pregnant with my other child, I stopped for a month, but it wasn’t successful. I had a miscarriage.” (Participant 3)
“My aunt-in-law was pregnant and used to drink alcohol. Her baby was born with very soft and flabby muscles. From what I can see, her baby looks sick and has very soft and flabby muscles. Maybe it’s the effects of alcohol.” (Participant 10)
Obtained information
Information from online media, laypersons, and healthcare providers also influenced participants’ understanding of harmful substances.
“I have read in some online papers that Ibuprofen should not be taken because it would affect the baby.” (Participant 2)
“I’ve read on the webpage that some medicines without prescription can affect the baby, causing yellow teeth or disability.” (Participant 1)
“In my opinion, although monosodium glutamate (MSG) is created specifically for cooking, my grandparents said that consuming too much MSG could cause hair loss or something like that.” (Participant 13)
“My mother has thyroid cancer and needs radiation therapy. I think that the radiation is harmful because the doctor tells me not to get close to my mother for seven days.” (Participant 9)
Theme 2: Practices for Safety
The participants performed their daily activities to attain safety through food safety, work safety, ambient air safety, and safety in personal/household products.
Food safety
Based on participants’ perceptions, eating was a specific activity in daily life, putting them at risk of involuntary and inevitable exposure to harmful substances. Food safety was attempted by choosing pesticide/chemical-free and organic food and safe containers (heat-resistant, non-styrofoam, plastic-free, and lead-free).
“I choose vegetables with worms and holes, meaning they have less pesticide. I also buy organic vegetables grown in the dome.” (Participant 14)
“I don’t use plastic or foam containers when it comes to hot food.” (Participant 2)
Some participants mentioned eliminating and reducing harmful residues such as washing, peeling, and heating and ceasing the consumption of prohibited food, beverages, and drugs without prescriptions.
“I think the pesticides are on the skin, so I wash and peel fruits before eating… I soak vegetables in salt water and wash several times, about three times.” (Participant 13)
“Before I got pregnant, I used to drink coffee, maybe 2-3 days a week. But once I got pregnant, I rarely drank it because the doctor said the baby would be small. I’m afraid it’ll harm the baby and cause a small baby size or low birth weight.” (Participant 3)
“When I have a fever, I tell the pharmacist that I am pregnant. I don’t buy drugs without a prescription.” (Participant 7)
Additionally, participants reduced consumption of some substances believed to be harmful, such as seasoning powder, food preservatives, growth boosters in chicken, red meat accelerating agents, bleaching agents, and formalin.
“Growth boosters for chicken, I am afraid they would negatively affect the baby. I rarely eat eggs. I eat about one egg a day, not many of them.” (Participant 13)
Work safety
Working environments potentially lead to harmful exposures. What participants could do included distancing, reducing, and using equipment, depending on their occupation. The health care provider mentioned X-ray avoidance by staying 2 meters away behind a thick wall.
“X-ray radiation doesn’t spread but remains on the floors, so I try to protect myself by staying away or staying behind something like a thick wall.” (Participant 8)
The fruit farmers chose to stop using the substances during their pregnancy. If not, they stayed away or upwind, refused to touch any contaminated areas or to eat on the farm, washed contaminated clothes separately, took a shower before eating, as well as put on long-sleeve shirts, shoes, masks, and a hat.
“When I come home from the farm contaminated with pesticides, I’ll rush to take a shower.” (Participant 1)
“When my husband applies the pesticides, I have to keep 50 meters distance. I try to stay upwind, wear a mask, and wear a long-sleeve shirt and long pants to the farm.” (Participant 13)
The office workers stayed or walked away after printers or photocopiers were working, moved the printer away from themselves, did not breathe in the printer smell, or asked someone else to switch duties.
“I have to make a lot of copies. There’s the fume from the printer’s toners. If I breathe it in, it won’t be good. Some radiations can cause miscarriage. So, I ask my male colleagues to photocopy for me. Sometimes I give an order to the machine to make photocopies, and I move away. When it’s done, I come to get the copies.” (Participant 9)
Cleaning staff in the hotel exposed to the smell of cigarettes and cleaning products asked for duty substitution:
“I’m exposed to cigarette smoke at work, in the guest rooms. If there’s a very strong smell when I enter the room, I’ll ask my colleague to clean the room for me.” (Participant 6)
Ambient air safety
Participants avoided harmful substances contaminated in the air environment, such as smoke from garbage burning, factories, cigarettes, and exhaust fumes. Air quality safety was achieved by several practices. Distancing included staying home, closing the house firmly, and relocating while eliminating or reducing was performed by covering the nose and holding breath.
“When they apply the pesticides around my house, I won’t leave. I would lock myself in the house. They have to apply pesticides for the durian and mangosteens next to my home, taking about 1-2 hours. I let them finish. I ask them how long they have finished. Then, I open the door and come out.” (Participant 1)
“When I walk in public places where people smoke, I’ll try to hold my breath and cover my nose with hands to avoid it as much as possible.” (Participant 8)
Moreover, those living in air pollution areas used equipment, including air purifiers, air conditioners, and fans.
“To avoid PM2.5, at home, I use an air purifier and turn on the air conditioner when I sleep.” (Participant 2)
“My husband likes to repair motorcycles, and there’s a smell of motor oil. I keep myself in the room with an air-conditioner. I don’t come out until he cleans the area.” (Participant 9)
Safety in personal/household products
Safe personal/household products, particularly for pregnant women, were unavailable, leading participants to choose less harmful products, such as baby or natural products; and to cease using unnecessary products, such as hair dyes.
“I choose baby products that have low acidity… It shouldn’t have many chemicals, unlike adult products. I think adult products may have more chemicals, but for the baby products, my baby can use them too.” (Participant 11)
“I had my hair dyed and straightened every two months. But when I realized I got pregnant, I don’t do it anymore.” (Participant 7)
Some participants tried to avoid direct contact with harmful household products as much as possible or had someone substitute them with household chores. Some avoided harmful household products by using equipment such as gloves if they had to use those products.
“Sometimes, I apply termite spray by myself, but I try to avoid direct contact as much as possible” (Participant 2)
“I try to prevent cleaning products from touching me or as little as possible. If there’re other people around, I’ll ask them to do it for me.” (Participant 3)
“For floor-mopping products, if contacting it directly, we must wear gloves.” (Participant 8)
Theme 3: Challenges in Avoiding Harmful Substances
Five challenges impeded the participants’ ability to be free from harmful substances.
Unrecognition
Lacking recognition of such harmful substances as arsenic, vitamin A for acne treatment, PM2.5, and dust prevented participants from properly avoiding them.
“I have never heard of arsenic. I don’t know it.” (Participant 14)
“Vitamin A? I don’t know it. I have never heard of it before.” (Participant 17)
“PM2.5…we don’t have it here, so I don’t pay much attention. I’m not sure about its effects on the baby or whether it’ll reach the baby, but it may affect us.” (Participant 12)
Unavailability of safe substances
Even if participants recognized the harm, safe products/food were unavailable and inaccessible in their community because the production processes were unknown, and the guarantee certification was unlikely presented on the products.
“I usually buy precooked meals at the market, but I don’t know the ingredients they use…whether the ingredients are safe or not.” (Participant 2)
“It’s difficult to avoid meat-enhancing agents. At department stores, there’re certifications and warranties, but I can’t go to department stores every day. I just go to the general market where nothing can be guaranteed.” (Participant 16)
Discomfort and inconvenience
The participants admitted to not using some protective equipment. For example, masks were not used because they caused difficulty breathing and discomfort. When applying fertilizers for their farms, participants did not put on gloves because they were inconvenient and time-consuming.
“When working on a farm, I don’t wear gloves because it’s not convenient. With gloves on, I have to be extra careful when holding a young cucumber plant because it may break or bruise.” (Participant 13).
“When going to the department store or the market, I never wear a mask. It feels uncomfortable, annoying, and makes me feel hot.” (Participant 15)
Inevitability
Work obligations and residence locations made the participants unable to prevent themselves from exposure. Household work led some participants to expose to some cleansing products for floors and bathrooms. The participants who worked as fruit farmers still used chemical fertilizers because it was their job. Other participants who were cleaning staff, healthcare providers, and office workers also cited that their jobs made them inevitably exposed to some harmful substances in their workplaces.
“It’s my occupation. We don’t hire anyone. My husband does it by himself. I have to help as much as I can. So, I might have had some exposure before I got pregnant. My husband has to care for the infected durian trees, so I have to help him apply the anti-disease substances.” (Participant 13)
Some participants lived in a contaminated area, surrounded by air pollutants, making avoidance impossible. This caused exposure to smoke from cigarettes, a rubber tree sawmill, burned garbage, fixing motorcycles, and using color spray and pesticides.
“My house’s surrounded by fruit farms. Although we don’t apply pesticides, our neighbors do. It may reach us because they apply it every other week.” (Participant 1)
Family traditions
Some participants had to share food with their families and ate what their families cooked or bought, which might not be safe for pregnant women. Some practices were their family tradition, such as food consumption in general and drinking tap or rainwater without a purification process, making them feel familiar and conform to those practices although they might doubt safety.
“Ground water’s been consumed by many generations in my family since my grandmothers. Now, I still live with my mother, so I drink whatever they drink without filtering or boiling. It should be alright because it’s consumed in our family. We’ve been using color-coated food containers for many generations. I use whatever they use. We don’t change things. I trust them; it shouldn’t be harmful.” (Participant 13)
Theme 4: Overcoming the Challenges
To safeguard their unborn baby from harmful substances, the participants made an effort to overcome the challenges in different ways.
Personal changes
To protect their unborn baby from harmful substances, participants changed their lifestyles and were more careful about everything. Drawing upon maternal instinct, participants gave up some habits for their unborn babies. They also tolerated certain symptoms as they tried to avoid exposing their unborn baby to medications.
“During pregnancy, I try to be more careful than before pregnancy because I’m afraid that there may be something that can harm my unborn baby.” (Participant 11)
“Once I got pregnant, I had to tolerate it, trying not to have a fever and sacrificing my beauty. Be careful about everything. I’m afraid that my baby will be born with a disability. I try to avoid bad things that can harm my baby.” (Participant 12)
“I think it’s an instinct. Most pregnant women wouldn’t care about their beauty. They wouldn’t visit beauty salons that would lead to the risk of inhaling substances during hair treatment or exposure to harmful substances from other clients.” (Participant 17)
Obtaining support
Besides making efforts of their own to overcome the challenges, it was crucial to obtain support from significant persons. Participants’ husbands, mothers, or mothers-in-law helped them by giving advice and warning, helping them to seek safe products and uncontaminated food, and even adjusting themselves. Furthermore, co-workers supported them by providing alerts and substituting duties.
“My mother warns me to stop drinking tea and coffee. She tells me not to eat pork and chicken because they have a lot of substances. It isn’t good for the baby.” (Participant 9)
“Before I got pregnant, my husband smoked, but when he knew it, he quit.” (Participant 15)
“Sometimes, my co-workers who had been pregnant warn me not to drink much tea. It’s not good.” (Participant 7)
“I ask my male co-workers to photocopy for me, and they do it.” (Participant 9)
When discussing the support from healthcare providers, participants unveiled that they received little information support, and there was no detailed explanation about harmful substances.
“Nurses just give me general information. They don’t ask me whether I have been exposed to harmful substances, what harmful substances I should avoid, or how they can affect my baby. Sometimes I don’t know the harmful chemical substances in food or daily products that I should avoid.” (Participant 5)
Since the obtained information was insufficient, participants had to search for more information on the Internet. Unfortunately, they doubted the reliability and accuracy of online information. Thus, they needed reliable information about harmful substances from healthcare providers.
“The knowledge received in the antenatal clinic doesn’t mention much about harmful substances. I usually search on the Internet and online pages, but not sure how reliable the information is. It’d be good to have a reliable manual about harmful substances that require precautions during pregnancy developed by health professionals.” (Participant 2)
Ensuring a peaceful mind
Participants mentally comforted themselves against fear and worried about an unborn baby’s health by keeping optimistic thoughts that exposure to harmful substances might not harm the baby. Moreover, they prayed based on their religions for blessing and protection for their unborn baby.
“If I have doubts, I’ll go to see a doctor, but I can’t go often if it’s not the appointment yet. I’ve no money, so I try to think positively and pray to Buddha’s image at home for my baby’s health.” (Participant 13)
“I’m worried like all other mothers. Based on my Christian beliefs, I pray to God to protect my baby so the baby’s born without disability. I pray to God every day.” (Participant 4)
Moreover, participants monitored their belly size and baby’s movement and underwent ultrasound or well-designed tests, which helped them feel relaxed.
“I might have been exposed to something harmful. I’m worried about the effect on the baby during the early pregnancy period. After the ultrasound, I feel more relaxed.” (Participant 2)
“At home, they came to apply termite spray. I felt worried, so I had a nifty test to examine the genes for any abnormality and Down syndrome.” (Participant 3)
Discussion
Our findings identified four major themes of the experiences of Thai pregnant women in their efforts to avoid harmful substances. The discussion was described in each theme, followed by limitations and implications of the study.
Theme 1: Understanding of Harms
In this theme, participants demonstrated an understanding that harmful substances possessed certain characteristics, such as unpleasant odors, corrosive properties, synthetic compositions, and the presence of waves or radiations. This finding aligns with a study conducted among female farmworkers (Flocks et al., 2012). Additionally, the participants believed that the severity of the effects on the unborn baby varied based on factors such as inhalation and consumption of the substances, as well as the quantity and frequency of exposure. Interestingly, this finding resonates with previous research where pregnant women perceived their alcohol consumption to be safe due to low and infrequent quantities consumed (Hammer et al., 2022).
Furthermore, the participants recognized that the impact of harmful substances on the baby depended on the elimination and accumulation of substances in the body and the protective mechanism (e.g., a placenta). While the placenta serves as a barrier between maternal and fetal circulations, regulating the transfer of teratogens from the maternal bloodstream (Cunningham et al., 2022), pregnant women still emphasize the need to prevent exposure to harmful substances, as some heavy metals can cross the placental barrier and reach the fetus (Molina-Mesa et al., 2022).
Participants also drew upon personal experiences of harm to themselves, others, or animals, as well as information obtained from various sources. Similarly, pregnant women drew upon their lived realities and previous pregnancies when determining the harms of alcohol consumption (Hammer et al., 2022), and their perceptions of harms were influenced by the popular media (internet, television, and magazines) and health professionals (Teysseire et al., 2019). Unfortunately, some harmful substances, such as vitamin A and arsenic, were not recognized due to the lack of previous experiences of exposure to such substances in their daily lives. Likewise, 90% of the Asian population in the United Kingdom did not know about arsenic contamination in rice (Mondal et al., 2019).
Importantly, none of the participants received health education on harmful substances and birth defects during antenatal clinic visits. This highlights the significant role that healthcare professionals, particularly nurses, can play in raising awareness among pregnant women about harmful substances in their daily lives. By gathering a history of previous exposures and providing tailored education based on each pregnant woman’s context, nurses can enhance pregnant women’s understanding and decision-making regarding harmful substances. This finding aligns with another study highlighting the need for personalized antenatal health education based on the diverse needs and contexts of pregnant women (Artieta-Pinedo et al., 2017).
Theme 2: Practices for Safety
This theme offered insights into the practices adopted by pregnant women to ensure their safety from harmful substances. In terms of food safety, participants engaged in practices such as choosing pesticide/chemical-free and organic food, using safe cooking utensils, reducing harmful residues through washing, and abstaining from consuming prohibited foods, beverages, and drugs without prescriptions. These practices align with recommendations to avoid fish high in mercury processed foods and to consume clean, fresh, and thoroughly-cooked food, as well as to wash vegetables and fruits and use clean cooking utensils (US Food and Drug Administration, 2022). Similarly, our findings are consistent with previous research indicating that pregnant women refrain from taking medicine without a prescription (Sychareun et al., 2022), reduce seafood consumption to minimize mercury exposure (Schaefer et al., 2019), and select safe food stalls and cooking utensils (Jevsnik et al., 2021).
Regarding work safety, participants exposed to harmful substances in their occupations implemented practices such as maintaining distance, reducing exposure, and utilizing protective equipment. These practices align with recommendations for work safety among pregnant women (National Institute for Occupational Safety and Health, 2023). Moreover, participants ensured ambient air safety by maintaining distance (e.g., staying at home, securely closing the house, and relocating) and reducing exposure (e.g., covering their noses and holding their breath). Similarly, pregnant women distance themselves from second-hand smoke exposure (Yavagal et al., 2021).
Regarding safety in personal and household products, participants opted for less harmful options such as baby or natural products and discontinued using unnecessary items like hair dyes. This aligns with findings from another study where women used organic products, moisturizers, or anti-stretch marks during pregnancy while refraining from using perfumes and deodorants (Sauvant-Rochat et al., 2019). Moreover, participants in our study reported ceasing the use of hair dyes (73%), insecticide sprays (72%), mosquito repellents (60%), and home renovation products (59%) (Teysseire et al., 2019).
Theme 3: Challenges in Avoiding Harmful Substances
The third theme revealed the challenges faced by pregnant women in avoiding harmful substances. One significant challenge was the participants’ lack of recognition of harmful substances, leading to inadequate avoidance practices. This finding aligns with another study that highlighted pregnant women’s unawareness of the adverse effects of second-hand smoke on pregnancy outcomes (Yavagal et al., 2021). It suggests that women may take proactive measures to minimize their exposure if they are aware of potentially harmful substances and effective strategies to limit exposure. This underlines the importance of educating women about the dangers of environmentally harmful substances and providing them with specific actions to reduce risky exposures.
Moreover, safe products were unavailable in the participants’ community, and their residence was in a community with high air pollution concentrations. Work obligations and adherence to family traditions also hindered pregnant women’s ability to avoid harmful substances. These challenges align with the experiences of Spanish pregnant women who faced pressures to disregard information on harmful substances due to their social and family situations, difficulties in balancing work and family responsibilities, higher prices of organic products, and limited accessibility to safe food (Fontalba-Navas et al., 2020). Unfortunately, participants in our study sometimes reported non-compliance with the use of protective equipment due to discomfort, despite being aware that their activities could involve exposure to harmful substances. Therefore, promoting pregnant women’s knowledge regarding the potential harm is crucial.
Theme 4: Overcoming the Challenges
This theme presented how participants overcame challenges in avoiding harmful substances through personal changes, obtaining support, and ensuring a peaceful state of mind. Participants demonstrated personal growth by adopting healthier behaviors, being more cautious, and making sacrifices driven by their maternal instincts. This aligns with the findings of Herzog-Petropaki et al. (2022), who found that pregnant women made significant changes in their health behaviors, such as abstaining from alcohol consumption and smoking, once they became aware of their pregnancy. Similarly, another study revealed that pregnant women refrained from alcohol consumption, motivated by their sense of maternal responsibility and prioritizing the well-being of their baby over personal desires (Hammer et al., 2022).
Notably, participants’ husbands played a supportive role by adjusting their habits to create a safe environment for pregnancy. For instance, husbands refrained from smoking, contributing to the overall health of the mother and the unborn baby (Firouzan et al., 2018). Therefore, involving family members in health education is crucial to enhance their supportive roles in ensuring the well-being of pregnant women. Evidence suggests that engaging husbands in health education increases their awareness of the risks posed by harmful substances to pregnant women, motivating them to actively modify their behaviors to create a safe environment for pregnancy (Soltani et al., 2019).
Another key finding is the need for increased professional support. Participants found that the information provided by health professionals was often general and lacked specificity regarding harmful substances, leading them to seek additional information online, which may be unreliable. Although pregnant women search for online information, they still require professional advice, considered the most reliable source (Obajimi, 2019). Thus, making self-learning materials available for pregnant women and developing clinical practice guidelines specifically addressing harmful substances is essential. However, the lack of specialized knowledge on environmental hazard prevention, limited proficiency in environmental health skills (Albouy-Llaty et al., 2019), and inadequate training in taking environmental health histories (Stotland et al., 2014) were reported. Therefore, training for nurses and other healthcare professionals is crucial to enhance their competency in addressing these concerns.
Furthermore, participants ensured a peaceful state of mind by maintaining optimistic views, seeking blessings through prayer, and undergoing regular examinations to monitor fetal health. These findings align with previous research that highlighted how pregnant women cope with concerns about congenital disabilities by relying on prayer, maintaining a positive mindset, and undergoing various diagnostic tests and sonography (Irani et al., 2019).
Limitations and Recommendations for Future Studies
This study provided the descriptive perspectives of pregnant women in southern Thailand, which might not represent pregnant women in other regions or contexts. Additionally, the participants were predominantly Buddhists, so that the findings may differ from pregnant women in other religions. Further research is recommended to explore the perceptions of pregnant women in other contexts to expand the generalizability of results.
Implications of the Study
There were several implications of this study for nursing practice based on the findings: First, nurses should receive training to educate pregnant women to raise their awareness of significant harmful substances found in daily life and promote effective practices to ensure safety in their daily activities. Second, nurses should be aware of the challenges pregnant women face in recognizing and avoiding harmful substances, address the lack of recognition of harmful substances, unavailability of safe products in the community, work obligations, and adherence to family traditions. Third, nurses should encourage and support pregnant women in making personal changes and obtaining support from their families, particularly husbands. Last, nurses can apply the findings to develop interventions for empowering pregnant women to overcome challenges through the engagement of family members and significant others in supporting and maintaining optimal surrounding that are safe from harmful substances for an unborn baby.
Conclusion
The pregnant women’s experiences with prenatal harmful substances revealed four themes, including the understanding of harms, practices for safety, challenges in avoiding harmful substances, and overcoming the challenges. The findings provide a sound understanding of prenatal harmful substances based on Thai pregnant women’s perspectives, which can be used as a foundation for developing comprehensive practice guidelines for antenatal health education suited to pregnant women’s culture and context.