Background
Fatigue is a prevalent concern among individuals undergoing continuous ambulatory peritoneal dialysis (CAPD). It refers to the feeling of tiredness or exhaustion, which can hinder the completion of tasks or the enjoyment of daily routines (Ream & Richardson, 1996). Scholars have highlighted that fatigue afflicts a substantial portion of dialysis-dependent patients, ranging from 70% to 85% (Almutary et al., 2016; Joshwa & Campbell, 2017; Tian et al., 2020). The experience of fatigue is often characterized as a persistent sense of a lack of energy, weakness, and exhaustion that persists despite periods of rest or sleep (James et al., 2020).
Fatigue has adverse effects across various dimensions of life among patients with CAPD. For instance, patients who experience high levels of fatigue engage in fewer daily activities and become more dependent on others (Abd-Rabouh et al., 2017). Several patients have expressed that fatigue significantly impacts their emotional well-being and social participation. Furthermore, others struggle to understand them when they attempt to explain the sensation of fatigue. Feeling fatigued restricts patients with CAPD from maintaining self-care routines, effectively managing their diet, or participating in social activities (van der Borg et al., 2021). Importantly, fatigue significantly predicts the mortality rate and increases the number of deaths (Guedes et al., 2022; James et al., 2020).
Several factors can influence fatigue among patients with CAPD, such as transferrin, alkaline phosphatase, total cholesterol, and sleep quality (Tian et al., 2020). Maruyama et al. (2021) reported that physical factors, including creatinine, body mass index, and age, were linked to the severity of fatigue. Psychological factors such as anxiety and depression were associated with fatigue in CAPD patients (van der Borg et al., 2021).
Considering the existing literature, researchers have predominantly concentrated on physiological and psychological factors that correlate with fatigue. These factors hinder nurses from comprehending and devising specific nursing interventions to alleviate fatigue. Therefore, exploring a range of factors manageable by nurses could significantly contribute to nursing care and its enhancement.
Nurses play a critical role in managing fatigue among these patients by assessing the severity of fatigue, delivering comprehensive nursing care to mitigate fatigue, and collaborating with a multidisciplinary team to ensure the entire healthcare team is engaged in the patient’s care. Hence, nurses need to comprehend the prevalence and evaluate potential factors contributing to fatigue within this population. Despite the examination of fatigue prevalence and factors among patients undergoing CAPD in foreign countries, certain aspects of those findings may not be directly applicable to the Thai context.
This expanding body of knowledge highlights the necessity for investigating the prevalence and influential factors related to fatigue among patients undergoing CAPD in Thailand. Consequently, our study aimed to explore: 1) the prevalence of fatigue and 2) the influencing factors (body mass index, duration since initiation of CAPD, insomnia, social support, functional status, depression) of fatigue among CAPD patients. The novel insights gained from this study regarding the prevalence and factors affecting fatigue in CAPD patients would aid nurses and other healthcare providers in accurately assessing and effectively managing fatigue in this population.
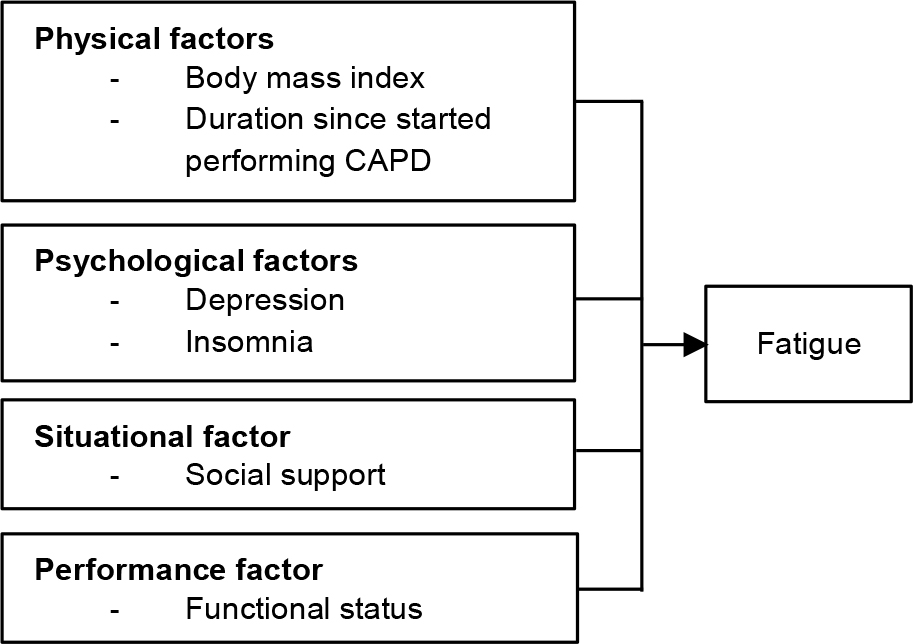
The Theory of Unpleasant Symptoms (TOUS), as proposed by Lenz et al. (1997), along with insights from the existing literature, served as the foundation for identifying the variables under study and shaping the conceptual framework. Lenz et al. (1997) delineated that the antecedents of symptom(s) consist of physical, psychological, situational, and performance factors, signifying that fatigue can arise from many aspects. Empirical evidence from Jhamb et al. (2019) revealed a correlation between higher body mass index in patients with end-stage kidney disease and increased fatigue. Prolonged dialysis treatment emerged as a primary contributor to depression and frustration, exacerbating feelings of fatigue (van der Borg et al., 2021). Patients reported high fatigue due to perceived limited support from family and friends (Garwai et al., 2020), while diminishing capacity to uphold functional status was associated with fatigue (van der Borg et al., 2021). Furthermore, patients undergoing CAPD who experienced sleep disturbances encountered heightened fatigue (Wang et al., 2016).
Given the insights from the extant literature, it is plausible to hypothesize that body mass index, duration since initiating CAPD, insomnia, and depression may serve as predictive factors of fatigue among patients undergoing CADP. The conceptual framework of this study is illustrated in Figure 1.
Methods
Study Design
This study employed a cross-sectional design.
Samples/Participants
The participants involved in this study were patients undergoing CAPD who visited the outpatient department of a general hospital in Thailand. The selection of participants was carried out using a purposive sampling technique. The inclusion criteria were: a) adults and older adults with confirmed chronic kidney disease undergoing CAPD, b) willingness to participate in the study, and c) ability to read and understand the Thai language. The participants who were designed to change the treatment option from CAPD to hemodialysis during the recruitment period were excluded.
The sample size calculation was performed using G*Power version 3.1.9.7. Referring to a prior study by Tian et al. (2020) that used a similar research design and investigated the same dependent variable, an effect size of 0.21, a statistical significance level of 0.05, and a test power of 0.80 was established. Consequently, the minimum sample size was 136. A six-region system was used to divide the geographical area of Thailand.
A stratified three-stage random sampling was employed to generate a probability-based sample of participants. In Stage 1, one region was chosen randomly from the six-region system, resulting in the selection of the central region. In Stage 2, one province was randomly picked from each of the chosen regions, leading to the selection of Nakhon Nayok province. In Stage 3, a simple random sampling was conducted to identify a general hospital within Nakhon Nayok province. Ultimately, Nakhon Nayok Hospital was designated as the data collection site for this study.
Instruments
Multiple instruments were used in this study. It is noteworthy that permissions to use all instruments were obtained from the original developers or copyright holders.
Demographic Data Form
The researchers developed this form and aimed to collect demographic data of the participants, including age, gender, marital status, education level, career, monthly income, duration of illness, comorbidity, and body mass index.
Fatigue Severity Scale (FSS)
The Thai version of FSS (Sawasdee et al., 2014) was employed to measure the severity of fatigue. Initially developed in English by Krupp et al. (1989), this 9-item scale required participants to select a number from 1 (strongly disagree) to 7 (strongly agree) that corresponded to their fatigue level. The total score for each item was determined by summing up the scores for the nine items and then dividing by 9. The total score ranged from 9 to 63. A cut-off score of ≥36 indicated the presence of fatigue. Hence, the total score was categorized into four groups: ≤36 (no fatigue), 36 – 45 (mild fatigue), 46 – 54 (moderate fatigue), and 55 – 63 (severe fatigue). The reliability of the FSS was previously assessed in patients with end-stage renal failure, yielding a Cronbach’s alpha coefficient of 0.93 (Bagheri-Nesami et al., 2016). In the current study, the reliability of the FSS, assessed through Cronbach’s alpha coefficients, was 0.79.
Center for Epidemiologic Study Depression Scale
The measurement of depression was conducted using the Thai version of the Center for Epidemiologic Study Depression (CES-D) Scale (Ploylearmsang, 2005), originally developed in English by Radloff (1977). The items retained in this scale specifically pertained to depression-related symptoms. This scale comprises 20 items and requires participants to rate each item on a scale from 0 (never) to 3 (often). The possible score range was from 0 to 60. A cut-off score of ≥16 indicated the presence of depressive symptomatology. The psychometric properties of this scale were previously examined in a study by Lau et al. (2023). In the present study, the reliability of the CES-D Scale was 0.71.
Multidimensional Scale of Perceived Social Support
Social support was assessed using the Thai version of the Multidimensional Scale of Perceived Social Support (Wongpakaran et al., 2011), originally developed by Zimet et al. (1990). This 12-item scale had three dimensions: family, friends, and significant others. Participants were instructed to rate their perceived social support level on a scale from 1 (strongly disagree) to 7 (strongly agree) for each item. The sum score ranged from 12 to 84, which was categorized into three levels: 12-36 (low), 37-60 (moderate), and 61-84 (high) for perceived social support. The psychometric properties of this scale were previously examined, confirming its validity and reliability in a study summarized by Shumaker et al. (2017). In the present study, the instrument’s reliability was 0.86.
Insomnia Severity Index (ISI)
The Thai version of ISI was employed to assess nighttime and daytime insomnia in this study (Keawphang & Jitpanya, 2004). Originally developed in English by Bastien et al. (2001), the ISI consists of 7 items, each rated on a scale of 0 to 4. The total score ranges from 0 to 28 and is categorized into four levels: 0-7 (no clinically significant insomnia), 8-14 (subthreshold insomnia), 15-21 (moderate insomnia), and 22-28 (severe insomnia) scores. The psychometric properties of the ISI were tested and led to the conclusion that it is a valid and sensitive measure for detecting insomnia (Bastien et al., 2001). In the present study, the reliability of the ISI was 0.76.
Functional Status Scale
The Functional Status Scale, developed by Maninet and Desaravinid (2023), was employed to assess an individual’s ability to engage in daily activities. This scale consists of 20 items, with three dimensions: physical activities (10 items), role and working activities (6 items), and psychological activities (4 items). Each item is rated on a scale from 1 (none of the time) to 4 (all of the time). The total score ranges from 0 to 80, and it is classified into three levels: 0 – 26 (low), 27 – 54 (moderate), and 55 – 80 (high) scores. The validity and reliability of this scale were assessed in a previous study by Maninet and Desaravinid (2023), and the instrument’s reliability was 0.87.
Data Collection
The researchers collected the data following the research protocol provided to the Nakhon Nayok Hospital’s human research committee. Data were collected between January and March 2023. Participants independently read and responded to the questionnaires. For older adults, researchers offered necessary explanations when required. On average, participants spent 30 minutes completing the questionnaires.
Data Analysis
Prior to the data analysis, the questionnaire responses underwent a thorough review and cleaning process. The Statistical Package for the Social Sciences (SPSS) software version 22 was utilized for data analysis. No outliers or missing data were identified. Participant characteristics were analyzed and described using percentages, means, and standard deviations. Categorical data was expressed through frequency and percentage. Pearson’s product-moment correlation analysis was employed to explore the relationships among body mass index, duration of starting CAPD, insomnia, social support, functional status, depression, and fatigue. Stepwise multiple regression was employed on the selected variables in the present study to evaluate predictive strength. The threshold for statistical significance was set at p <0.05.
The assumptions of the multiple regression analysis were assessed. To determine linearity, scatterplots were employed to examine the relationships between each independent and dependent variable, revealing linear associations among all pairs. Pearson’s product-moment correlation analysis was used to assess the relationships between the independent variables, showing correlations below 0.33. Additionally, normal probability plots were inspected, confirming the normal distribution assumption for all variables under investigation. Thus, the multiple regression analysis was appropriate for this study.
Ethical Considerations
The Nakhon Nayok Hospital’s human research committee granted approval for this study on 23 January 2023 under reference number REC No 17/2565. Contact was established with participants to obtain their consent for participation. The study’s objectives, research design, potential risks, and benefits were thoroughly explained. All participants were given the right to withdraw from the study until the data collection was concluded. Subsequently, all participants provided formal consent and signed consent forms prior to their enrollment in the study.
Results
Characteristics of the Participants
This study achieved a 100% participation rate among the participants. Table 1 presents an overview of the participants’ characteristics in this study.
| Variable | n | % |
|---|---|---|
| Age (years) | ||
| 30 – 59 | 88 | 64.71 |
| ≥60 | 48 | 35.29 |
| Gender | ||
| Male | 77 | 56.60 |
| Female | 59 | 43.40 |
| Marital Status | ||
| Married | 105 | 77.20 |
| Single | 17 | 12.50 |
| Divorced | 14 | 10.30 |
| Education Level | ||
| Primary school | 98 | 72.10 |
| High school | 7 | 5.10 |
| Junior high school | 12 | 8.80 |
| Diploma degree | 5 | 3.70 |
| Bachelor or higher degree | 3 | 2.20 |
| Uneducated | 11 | 8.10 |
| Household Monthly Income (Thai Bath) | ||
| 0 – 10,000 | 109 | 80.15 |
| 10,001 – 20,000 | 23 | 16.91 |
| 20,001 – 30,000 | 4 | 2.94 |
| Duration Since Started Performing CAPD (Months) | ||
| 1 - 24 | 90 | 66.18 |
| 25 - 48 | 15 | 11.02 |
| 49 - 72 | 24 | 17.65 |
| 73 – 96 | 5 | 3.68 |
| 97 – 108 | 2 | 1.47 |
The participants’ average age was 56.82 years (Standard deviation: SD = 8.92), ranging from 30 to 74 years. The mean duration of CAPD performance was 26.41 months (SD = 25.94), ranging from 1 to 107 months. The average body mass index was 18.79 kg/m² (SD = 2.62), ranging from 13.75 to 27.27 kg/m². Moreover, the majority of participants were male (56.60%), married (77.20%), had completed primary school (72.10%), and were engaged in agriculture (41.90%). While most participants did not have any comorbidities (64%), a smaller proportion had been diagnosed with diabetes mellitus (16.20%), hypertension (10.30%), both diabetes mellitus and hypertension (4.40%), heart disease (3.60%), and gout (1.50%), respectively.
Prevalence of Fatigue among Patients Undergoing CAPD
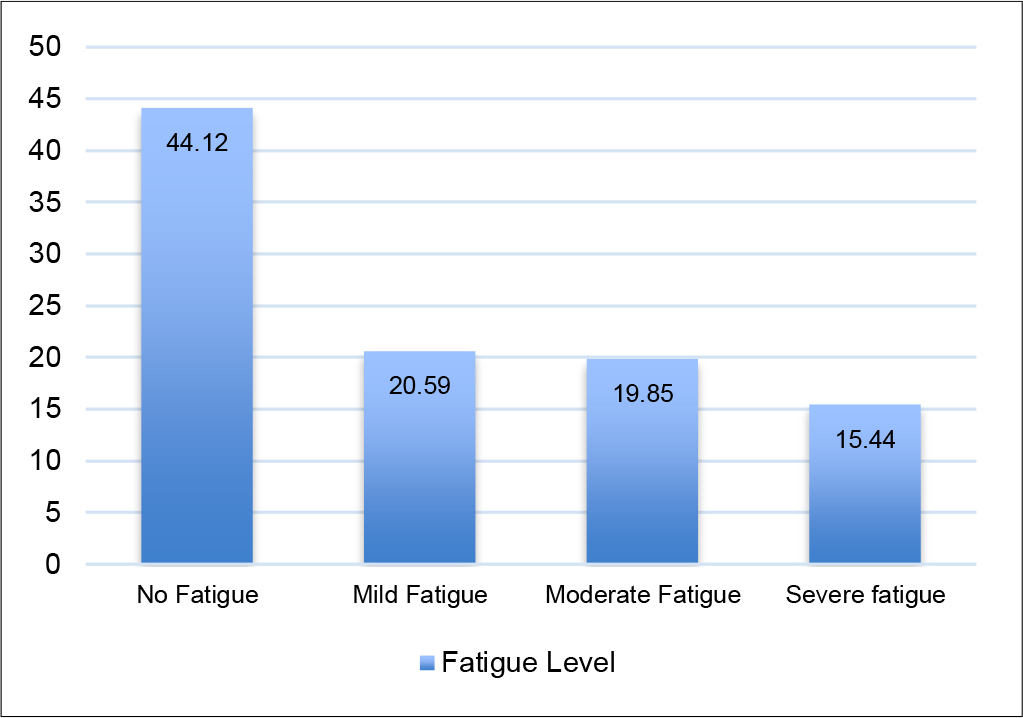
The findings of this study revealed that 55.88% of the participants reported experiencing fatigue, with categorizations including mild fatigue (20.59%), moderate fatigue (19.85%), and severe fatigue (15.44%). The mean fatigue score was 36.07 (SD = 16.74). However, 44.12% of the participants had no fatigue. Figure 2 visually illustrates the various levels of fatigue among patients undergoing CAPD in this study.
Factors Related to Fatigue: Bivariate Analysis
As presented in Table 2, Pearson’s product-moment correlation analysis revealed that five independent variables were significantly related to fatigue among patients undergoing CAPD. Insomnia (r = 0.578, p <0.01), depression (r = 0.408, p <0.01), and body mass index (r = 0.239, p <0.01) had significantly positive correlations with fatigue. On the other side, social support (r = -0.468, p <0.01) and functional status (r = -0.313, p <0.01) had significantly negative correlations with fatigue among patients undergoing CAPD.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Duration of stating CAPD | 1 | ||||||
| 2. Body mass index | -0.158 | 1 | |||||
| 3. Depression | 0.027 | 0.158 | 1 | ||||
| 4. Insomnia | -0.100 | 0.328** | 0.329** | 1 | |||
| 5. Social support | 0.007 | -0.237** | -0.164 | -0.274** | 1 | ||
| 6. Functional status | 0.095 | -0.050 | -0.176* | -0.204* | 0.157 | 1 | |
| 7. Fatigue | -0.079 | 0.239** | 0.408** | 0.578** | -0.468** | -0.313** | 1 |
Factors Influencing Fatigue: Multivariate Analysis
The multiple regression analysis revealed that several factors influenced fatigue among patients undergoing CAPD. Specifically, insomnia (β = 0.399), social support (β = -0.302), depression (β = 0.201), and functional status (β = -0.149) emerged as significant predictive factors of fatigue. Collectively, these four factors accounted for 50.10% of the variability in participants’ fatigue levels. Further information is presented in Table 3.
| Variable | B | SE | Beta (β) | t | p-value |
|---|---|---|---|---|---|
| (Constant) | 63.171 | 8.864 | 7.126 | <0.001 | |
| Insomnia | 0.780 | 0.133 | 0.399 | 5.880 | <0.001 |
| Social support | -0.463 | 0.099 | -0.302 | -4.671 | <0.001 |
| Depression | 0.354 | 0.116 | 0.201 | 3.042 | 0.003 |
| Functional status | -0.203 | .087 | -0.149 | -2.339 | 0.021 |
| R = 0.708, R2 = 0.501, SE = 11.991, F(4, 131) = 32.871, p <0.001 | |||||
Discussion
In this study, fatigue was reported by 55.88% of the participants. The bivariate analysis indicated that fatigue-related factors among patients undergoing CAPD were insomnia, depression, body mass index, social support, and functional status. However, the multiple regression revealed that only insomnia, social support, depression, and functional status influenced fatigue among patients undergoing CAPD, which collectively accounted for 36.80% of the observed variance. Several aspects warrant discussion concerning the objectives of this study, which are outlined as follows.
In terms of fatigue prevalence, this study discovered that more than half of the participants experienced fatigue. This observation highlights the common occurrence of fatigue among patients undergoing CAPD. When comparing our findings to existing literature, the prevalence of fatigue found in this study aligns with the results of Garwai et al. (2020), who reported a fatigue prevalence of 60% among patients undergoing CAPD. Other studies have documented even higher rates of fatigue in patients undergoing CAPD. For instance, Tian et al. (2020) identified that 78.70% of peritoneal dialysis patients in China experienced varying degrees of fatigue severity. Similarly, another study reported that up to 88.50% of CAPD patients encountered fatigue, potentially impacting their ability to perform daily tasks effectively (Maruyama et al., 2021).
Several factors could contribute to the comparatively lower fatigue rate observed in the current study. One possibility is that participants perceived better support from their social circles, including family members and friends (mean = 72.04, SD = 10.91), which could contribute to reduced fatigue. Furthermore, a significant proportion of participants in this study were married (77.20%). Within Thai culture, marital status holds considerable value and respect. This cultural aspect might play a role in spousal responsibility, where partners take on caregiving tasks such as meal preparation and laundry for their loved ones dealing with long-term health conditions. As a result, this support system could conserve patients’ energy and alleviate fatigue.
Interestingly, 44.12% of the participants in this study reported being free from fatigue. This observation indicates that not all patients undergoing CAPD encounter fatigue. This phenomenon prompts an exploration of factors contributing to the absence of fatigue in certain patients. Firstly, the mean body mass index (BMI) of the participants in this study was 18.79 kg/m² (SD = 2.62), indicating a normal level. Gao et al. (2021) emphasized that CAPD patients with a normal BMI tend to experience reduced fatigue due to their adherence to a well-regulated diet and effective fluid management, which is essential for maintaining optimal energy levels. Secondly, the majority of participants were male (56.60%). This observation suggests that males may naturally possess heightened adaptability and physical well-being compared to females. This premise is supported by a study conducted in the United Kingdom, which revealed a significant gender-based difference in fatigue reporting (p <0.05). The study identified a greater proportion of fatigue among females (Al Naamani et al., 2021).
Regarding the factors related to fatigue among patients undergoing CAPD, this study, based on bivariate analysis, revealed that insomnia, depression, and body mass index were positively associated with fatigue. These findings align with previous research (Brys et al., 2020; Kim et al., 2019; Wang et al., 2016), all of whom reached similar conclusions. For instance, Kim et al. (2019) and Wang et al. (2016) highlighted the link between insomnia and fatigue among patients undergoing CAPD, positing that insufficient sleep can contribute to heightened feelings of fatigue.
Concerning the relationship between depression and fatigue, the study result aligns with Brys et al. (2020), who observed an association between depression and fatigue among individuals with chronic kidney disease. One possible explanation for this finding is that depression may exacerbate fatigue by diminishing motivation and hindering activity engagement. Additionally, depression can impact personal physical and emotional energy levels, further contributing to fatigue. Consequently, patients with CAPD who grapple with depression often contend with heightened fatigue and challenges in daily activities (Thangarasa et al., 2018).
Furthermore, this study is the first to establish a correlation between body mass index and fatigue among patients undergoing CAPD. This finding suggests that participants with higher body weights might struggle with elevated fatigue levels throughout the day. Additionally, carrying extra weight could strain the body more, resulting in overall tiredness and reduced energy levels.
Social support and functional status had a significant negative correlation with fatigue among patients undergoing CAPD. This highlights that patients undergoing CAPD who receive enhanced social support from family, friends, or healthcare personnel tend to report lower fatigue levels. In the context of Thailand, the provision of support by family members and friends seems particularly effective in mitigating fatigue in CAPD patients (Polsingchan & Rungruang, 2022). Family members play a pivotal role in offering patients a sense of comfort, empathy, and understanding, thereby reducing feelings of fatigue. However, this study’s finding contrasts with that of Garwai et al. (2020), who conducted a cross-sectional study on patients undergoing hemodialysis and reported a positive association between social support and fatigue (p = 0.02). Additionally, another study highlighted that patients undergoing peritoneal dialysis experienced a decline in social support over the course of the disease and dialysis period, expressing inadequate support from spouses, friends, and children (Avdal et al., 2020).
Functional status had a significant negative correlation with fatigue among patients undergoing CAPD, implying that individuals with higher functional status experience less fatigue. While a prior study discovered a correlation between fatigue and functional status in older patients undergoing hemodialysis (Abd-Rabouh et al., 2017), an alternative interpretation suggests that reduced capability to perform routine daily functions could elevate the risk of experiencing high fatigue levels.
Interestingly, this study found no association between the duration since starting CAPD and fatigue. This suggests that despite the need for patients undergoing CAPD to perform the procedure multiple times a day, often at specific intervals, to maintain their fluid and electrolyte balance, it did not result in feelings of fatigue. This might be because the long-term experience performing CAPD could enhance the ability to achieve sufficient dialysis clearance. A study by van der Borg et al. (2021) supported this, indicating that patients who have been on CAPD for an extended period have developed a better comprehension of their treatment and improved coping mechanisms. Consequently, they can effectively adhere to the description of CAPD in terms of waste product and excess fluid clearance (van der Borg et al., 2021).
However, in our study, based on multiple regression analysis, the findings unveiled the independent variables, specifically only four—insomnia, social support, depression, and functional status—significantly influenced fatigue among patients undergoing CAPD, contributing to 50.10% of the variance within this patient population. In the context of the Theory of Unpleasant Symptoms (Lenz et al., 1997), these outcomes further validate the role of physical, psychological, and situational factors in influencing fatigue within this cohort. Insomnia, a sleep disorder characterized by difficulty falling asleep, emerged as a prominent factor closely associated with fatigue among this group. This observation aligns with the findings of a prior systematic review and meta-analysis study, which highlighted a high prevalence of insomnia in conjunction with higher levels of fatigue among individuals with chronic kidney disease (Tan et al., 2022). Moreover, another study revealed a positive correlation between depression and insomnia (Liu et al., 2021), and depression elucidated up to 46% of the variance in fatigue among patients undergoing peritoneal dialysis (Liu et al., 2021). Consequently, patients undergoing CAPD grappling with insomnia might potentially encounter heightened levels of depression and fatigue.
Furthermore, a decline in functional status can consequently impact the experience of fatigue. Existing evidence has indicated that patients with chronic kidney disease often face challenges in terms of poor functional status, which manifests as difficulties in carrying out fundamental activities of daily living such as dressing, grocery shopping, and driving (Modesto et al., 2018). Without support from family, friends, and significant others, this population has unpleasant symptoms and low quality of life (Shah et al., 2018). Thus, these four variables—insomnia, social support, depression, and functional status—emerge as pivotal determinants with the potential to influence the experience of fatigue among patients undergoing CAPD.
Limitations of the Study and Recommendations for Future Research
There are a few limitations in this study. The utilization of participants from a singular setting may hinder the generalizability of the findings to a broader population across Thailand. Moreover, it is essential to acknowledge that, in line with the theory of unpleasant symptoms, only limited factors can be explained in the linkage between physical factors, psychological factors, situational factors, and symptoms.
For future research, it is suggested to conduct screenings utilizing standardized instruments to identify participants experiencing fatigue. This approach could contribute to a comprehensive depiction of the fatigue phenomenon among patients undergoing CAPD. More studies exploring the factors related to fatigue among this population are needed. In addition, further research would be valuable to explore the potential causal interplay between insomnia, social support, depression, functional status, and fatigue within the context of patients undergoing CAPD. Furthermore, an investigation comparing the prevalence of fatigue among patients with end-stage renal disease undergoing diverse treatments such as CAPD, hemodialysis, and kidney transplant throughout Thailand warrants exploration. Additionally, the development of nursing interventions with a specific focus on fatigue management could be a fruitful avenue for further inquiry.
Implications of the Study for Nursing Practice
This study’s findings offer several avenues for integrating into nursing practice to enhance patient care. Nurses play a pivotal role in comprehending the distinctive attributes of fatigue experienced by patients undergoing CAPD. The identified prevalence highlights the significance of nurses routinely evaluating fatigue severity. This assessment strategy can include both vigilant observation and the utilization of standardized assessment tools. Additionally, it is essential to establish open lines of communication between patients, their families, and healthcare providers to address fatigue-related concerns. Furthermore, a proactive exploration of potential fatigue-inducing factors is warranted. This study highlights the potential benefits of interventions aimed at improving rest and sleep quality, effectively managing depression, fostering social support, and enhancing functional status. By implementing these strategies, nurses can contribute significantly to managing and mitigating fatigue among patients undergoing CAPD.
This newly acquired knowledge holds the potential for refinement and integration into nursing interventions aimed at fatigue management. Implementing healthcare education sessions that include strategies for alleviating fatigue among patients undergoing CAPD is advisable. For instance, emphasizing the importance of achieving restful sleep is vital. Patients with CAPD should aim for 7-8 hours of uninterrupted sleep per night and establish a consistent bedtime routine. When encountering signs of depression or other medical conditions contributing to fatigue, seeking guidance from nurses or healthcare professionals is encouraged.
Moreover, regular physical activity can effectively diminish fatigue and boost overall energy levels. Patients undergoing CAPD can contemplate integrating low-impact exercises such as walking, cycling, or swimming into their daily regimen. It is essential, however, to customize these approaches according to individual patient needs and preferences. Seeking input from a multidisciplinary team can offer valuable insights for tailoring these strategies effectively.
Conclusion
Fatigue is common among patients undergoing CAPD. This study highlights the essential and imperative nature of evaluating fatigue within this patient group. Within the framework of the theory of unpleasant symptoms, insomnia, social support, depression, and functional status emerge as pivotal factors that influence fatigue levels. Consequently, nursing interventions to mitigate fatigue among CAPD patients should prioritize strategies for enhancing sleep quality, alleviating depression, enhancing physical activity, and actively involving family members in the care program.