Background
In Thailand, morbidity from type-2 diabetes mellitus (T2DM) is expected to increase to 6,066.6 per 100,000 by 2045 (International Diabetes Federation, 2021). Diabetes is the 10th leading cause of premature mortality in Thailand, resulting in 747,000 deaths in 2021 (International Diabetes Federation, 2021). Moreover, T2DM will lead to acute and chronic complications (Thai Ministry of Public Health, 2023). A diabetic foot ulcer is a chronic complication that frequently appears and usually results in foot infections and eventual lower extremity amputation (LEA) in cases involving no foot ulcer treatment or prevention (Thai Ministry of Public Health, 2023). In addition, the average healthcare cost from T2DM trends increases, resulting from diabetic complications, especially when hospitalization is necessary because of complications that have arisen (International Diabetes Federation, 2017). However, complications can be prevented through improved lifestyle modifications and the administration of foot care (Corbett et al., 2019) through collaboration between healthcare providers as nurses and patients with diabetes (PWDs).
Based on the complexity of T2DM and its complications, PWDs require continuing care to reach optimal outcomes effectively (ElSayed et al., 2023b). Those patients are not only hospitalized but also return to their homes to manage their health, including lifestyle modification through a collaboration between PWDs and the healthcare system (ElSayed et al., 2023b). Therefore, self-management was developed (Ryan & Sawin, 2009). Nurses can help promote diabetes self-management (Kanan et al., 2018; Koetsenruijter et al., 2016). Over the past decade, nurses have mainly educated patients on foot care to delay such complications or foot ulcers. However, this given information is provided as a one-way communication strategy; for example, nurses instruct those patients without exactly focusing on backward feedback or patients’ needs, resulting in those nurses not hearing the patients’ voices. There were times when the information given by those nurses did not match the needs of the patients. Hence, person-centered care is a priority recommended by the American Diabetes Association (ADA) because effective patient-physician/nurse communication is one aspect of enhanced diabetes self-management, leading to a better quality of care (ElSayed et al., 2023b).
According to a literature review, previous studies relating to PWDs have shown limited attention to their needs for foot care and foot-complication prevention in Thailand, while such care and prevention have mostly been studied in developing countries (Nang et al., 2019; Ugwu et al., 2020). Applying the results of such a study might make a difference in the Thailand healthcare system. Currently, in Thailand, diabetes self-management remains low (Boonsatean et al., 2018), especially in foot-care self-management (Kanan et al., 2018). Furthermore, there has been a mismatch between standard foot care and the patients’ needs for a long time. To understand the needs of patients for the prevention and treatment of their foot complications is essential. The use of a qualitative descriptive approach might contribute to the ability of the nurses in their efforts to modify their nursing care in such a way as to match the needs of their patients as much as possible since a qualitative descriptive philosophy is meant to understand a factual situation as it occurs in a natural setting (Sandelowski, 2000). Accordingly, this qualitative descriptive study focused on exploring the needs of PWDs in preventing and treating foot complications. Therefore, those needs require the provision of preliminary information for modifying education strategies, foot-care services, and clinical guideline development.
Methods
Study Design
This qualitative descriptive study intended to explain the prevention and treatment needs of PWDs with foot complications who were visiting the Surgical and Diabetic Foot Excellence Center at the university hospitals of Thailand. A qualitative descriptive approach is crucial to understanding a factual situation as it may occur in a natural state (Sandelowski, 2000) so that the principal investigator (PI) can directly obtain the data from the participants. This study was written based on the COnsolidated criteria for REporting Qualitative research (COREQ) checklist (Tong et al., 2007).
Participants
A purposive-sampling method based on five-foot ulcer risk classification, consisting of 30 participants, was used for PWDs as a low-risk group PWDs without foot complications and diagnosed with T2DM for at least two years with full consciousness, orientation, and good Thai communication skills); for PWDs as a mild-risk group (PWDs with peripheral neuropathy (PN)/ peripheral vascular disease (PVD) and without foot ulcers/lower extremities amputation (LEA) who had been diagnosed with T2DM for at least two years with full consciousness, orientation, and good Thai communication skills); and for PWDs as a high-risk group (PWDs with full consciousness, orientation and good Thai communication skills with a) at least one hospitalization caused by diabetic foot ulcer (DFU) with full healing; b) recurrent DFU; and c) LEA). Withdrawal or termination criteria included PWDs who wished to withdraw during the study. No participants withdrew at the end of the data collection.
Data Collection
Data collection was performed after receiving permission from the ethical committee between June and July of 2021 at the health promotion center, Faculty of Nursing, Thammasat University, Thailand. The PI moderated over 40-minute focus group discussions (FGDs) in each of the five groups with four semi-structured questions developed on the basis of a literature review (Merighi et al., 2013; Papaspurou et al., 2015; Quandt et al., 2013), including one introductory question, two focus questions (health issues, barriers to foot care), and a summary question. After a semi-structured interview guide was developed, the PI performed content validity with three qualitative experts, and then the PI corrected those semi-structured questions following qualitative experts’ suggestions with a 1.0 content validity index before submitting them to the ethical committee. Also, FGD is a data-gathering method in this study for exploring a specific topic of interest in a broad spectrum of the participants’ experiences and viewpoints. In addition, FGD is suitable for understanding different and similar viewpoints, the new ideas of those participants, or approving concepts/hypotheses (INTRAC, 2017). The purpose of FGD is mainly to understand the participants’ opinions, feelings, and behaviors (INTRAC, 2017). The FGD was operated by the PI at different times (one by one) for each group based on a meeting schedule. Based on the data-collection process, the PI used various methods (field notes, an interview guide, an audio electronic recorder) for trustworthiness and different data collection times for creditability. During a group discussion, the PI established a relaxed, open, and trusting atmosphere in a private room and a beginning professional relationship among the participants, taking 5-10 minutes. The PI had them sit in a circle, thus providing ample space for their body movement during the discussion, and prepared a non-sweetened beverage for them. The PI used an audio recording device with the participants’ permission, and the research assistant took field notes.
Data Analysis
Manual content analysis based on the Miles and Huberman principle was used for data analysis (Miles & Huberman, 1994) as follows: 1) verbatim transcription within 24 hours after the interview; 2) data categorization by the PI and one research team; for example, those researchers carefully read every sentence related to the research questions, because each sentence represented the coding. Each coherent statement was rearranged as an open coding. Then, the PI and one research team reread the qualitative data for naming and grouping as axial coding. The PI and one research team analyzed, discovered, and described each code. The PI and one research team reread each sample of raw qualitative data for conflict discovery with bias avoidance. Last, a conclusion drawing/verification was performed.
Trustworthiness
Data triangulation and member checking were used for trustworthiness based on Lincoln and Guba’s principles (Lincoln & Guba, 1985). The research team needed to involve the participants’ voices for members checking in the content analysis and interpretation through cell phones, aiming at refraining from the researchers’ biases. Data collection methods (field notes, semi-structured interviewing guide, and audio recording files) and careful timing were used for data-coherence checking. In addition, PWDs with a 5-foot-level ulcer-risk classification were used for purposive sampling (Teddlie & Yu, 2007). Furthermore, the PI took the necessary time needed to build a professional relationship, which was around 5-10 minutes before interviewing and observing, which was supplemented with field note-taking by the research assistant for credibility. In order to assure trustworthiness, this study also used field notes to record the atmosphere or interactions of those participants during FGDs and used them to recheck any emerging themes for verbatim transcription. The details of the field notes obtained were consistent with those themes. The qualitative data were systematically collected and stored for verification (Lincoln & Guba, 1985). In this study, data collection was conducted in a private room at the health promotion center at the Faculty of Nursing, Thammasat University, based on meeting schedules. For systematic data collection, the PI kept audio files on the PI’s computer with password protection so that nobody could access them without permission from the PI. According to data stored for verification, paper documentation was kept in a locked cabinet in the PI’s office, and all data were held for all stakeholders’ verification (e.g., participants, research teams, and the Ethical Committee). Two researchers separately read, coded, and grouped the emerging themes, and findings were grouped and summarized (dependability) (Lincoln & Guba, 1985). Finally, the emerging themes were rechecked with a qualitative specialist and the participants for confirmability.
Ethical Considerations
This study was approved by the Ethical Committee (No.1), Faculty of Medicine, Thammasat University (MTU-EC-OO-6-134/62). The study conformed to the ethical guidelines for human subjects. The PI used inclusion and exclusion criteria for sampling at the surgical unit and Thammasat University Center of Excellence for Diabetes Foot Care Center (TU-CDC). The PI introduced herself to tentative participants and explained the research objective and the advantages of participation. After informed consent had been received, the PI collected data within 40 minutes of each FGD in a private room at the health promotion center, Faculty of Nursing, Thammasat University, next to both surgical deportment and TU-CDC. Both consent and data-collection processes took place in a private room at this center. According to the informed-consent process, the participants were informed with explanations regarding their right to withdraw from this study at any time. At the conclusion of a group discussion, the data and paper-and-pencil documents were stored confidentially in a cabinet with a key at the PI office, and their confidentially remained throughout this study. Audio electronic files were kept in the PI computer with passwords so that they could not be accessed by anyone not authorized. Both audio electronic files and other documentation were deleted from all sources and destroyed by a paper shredder within five years of completing the data collection.
Results
Characteristics of the Participants
The ages of the participants ranged from 33 to 82 years old. A majority of the participants were unemployed (36.63%) and had a family history of T2DM (73.33%), affecting first-degree relatives (86.36%). The average T2DM duration was 13.21 years, and the average A1C was 8.08%, while 83.25% received the combined treatment (Table 1).
| Characteristics | f | % |
|---|---|---|
| Sex | ||
| Male | 15 | 50 |
| Female | 15 | 50 |
| Age (Year) | M = 59.5; Range = 33-82 | |
| Marital status | ||
| Married | 20 | 66.67 |
| Divorced | 5 | 16.67 |
| Single | 5 | 16.67 |
| Number of children | M = 1.96; Range = 1-4 | |
| Education level | ||
| Elementary school | 12 | 39.96 |
| High school | 5 | 16.65 |
| Vocational certificate | 1 | 3.33 |
| Bachelor’s degree | 10 | 33.33 |
| Master’s degree | 2 | 6.66 |
| Occupation | ||
| Unemployed | 11 | 36.63 |
| Merchandise/business | 6 | 19.98 |
| Retired civil servants | 6 | 19.98 |
| Hired workers | 3 | 9.99 |
| Civil servant/state enterprises | 3 | 9.99 |
| Agriculture | 1 | 3.33 |
| Family history of T2DM | ||
| Yes | 22 | 73.33 |
| ◦ First degree | 19 | 86.36 |
| ◦ Second degree | 3 | 13.63 |
| No | 8 | 26.67 |
| Diabetes duration (Year) | M = 13.21; Range = 3-30 | |
| Glycemic control | ||
| A1C | M = 8.08%; Range = 5.6-11.8 | |
| FBS | M = 153.23 mg%; Range = 76.05 – 312.98 | |
| Treatment plan | ||
| Dietary control only | 0 | 0 |
| OHA only | 3 | 9.99 |
| Insulin only | 1 | 33.33 |
| Combined | 25 | 83.25 |
| Others: exercise, herbal | 1 | 3.33 |
| Medical rights | ||
| Civil-servant medical benefits | 14 | 46.62 |
| UHC | 6 | 19.98 |
| Social insurance | 4 | 13.32 |
| Cash | 3 | 9.99 |
| Handicap | 1 | 3.33 |
| Elderly services | 1 | 3.33 |
| Others | 1 | 3.33 |
Note: FBS, fasting blood sugar; OHA, oral hypoglycemic agent; UHC, universal healthcare; M = Mean
Thematic Findings
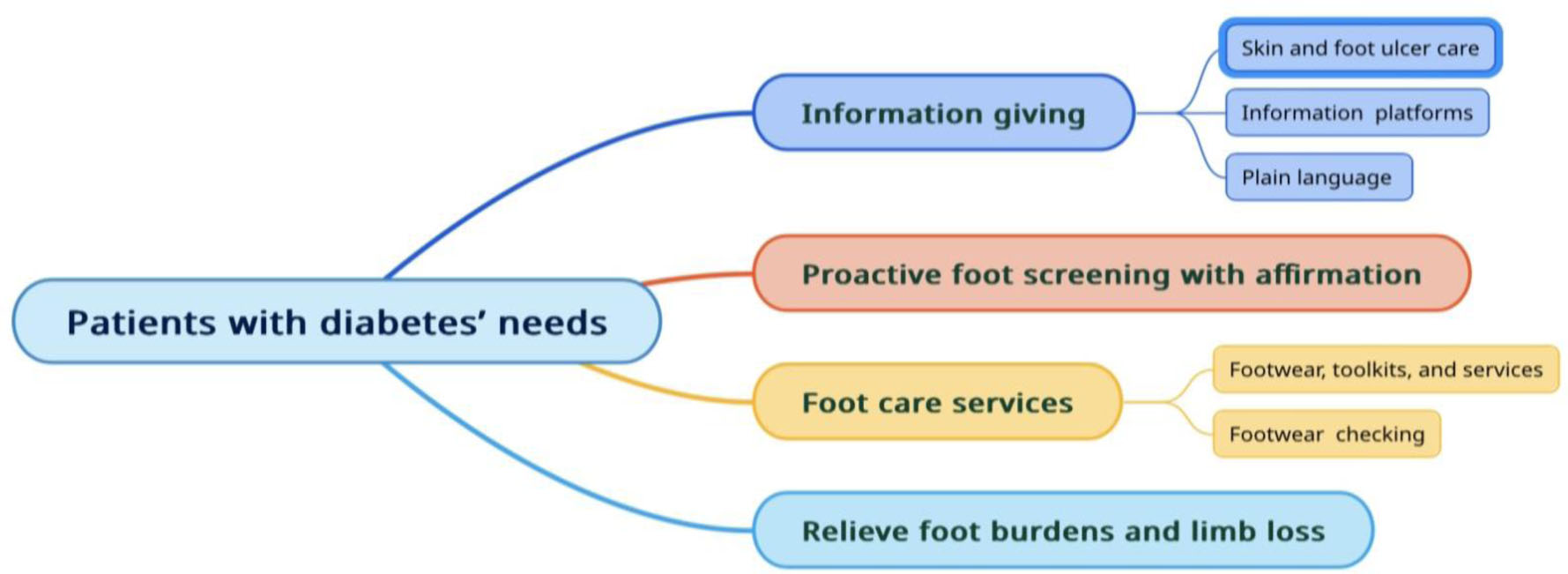
Based on the emerging themes, most needs are similar in each risk group, especially in the low-risk and moderate-risk groups. However, some of the participants in moderate and high-risk groups provided different themes, which might be caused by the changing needs of patients over time. Four themes of patients’ needs regarding foot complication prevention and treatment emerged: 1) information giving, 2) proactive foot screening with foot-care affirmation, 3) foot care services, and 4) relieving foot burdens and limb loss (Figure 1).
Theme 1: Information Giving
Participants indicated that the foot care/foot ulcer care information and platforms available to each patient were inadequate in terms of lack of access to information in provincial hospitals, resulting in a foot care barrier. In addition, using technical terms during the delivery of information made the information difficult to understand.
Subtheme 1.1 Increased information with in-depth detail regarding skin problems and foot ulcer care
Most of the participants stated that they prefer nurses to provide them with information regarding the causes of skin problems (e.g., dry skin and itchy skin) as well as skincare to relieve these discomforts. The participants requested more information about foot ulcers and more details about foot ulcer management. In addition to care instruction, foot care should be trained as quoted below:
“(Nurses) told me that (I) should not scratch (itchy skin)…how do I deal with it (itchy skin)…I used to apply urea cream, but it didn’t relieve it…so, I still need to scratch it.” (Participant 1, male, A1C 7.3%, a low-risk group)
“Need instructions for itchy skin…what causes (itchy skin)…I want to know about the causes.” (Participant 3, female, A1C 8%, a low-risk group)
“(My skin) is very itchy. How can I take care of dried skin?” (Participant 6, female, A1C 9%, a low-risk group)
“When I have a wound, how can I deal with it” (Participant 22, female, A1C 9%, a high-risk group)
Subtheme 1.2 A various information platform
Participants highlighted inadequate foot care information in some of the hospitals in Thailand where they were referred and information inaccessibility. The participants’ quotes can be seen below:
“A provincial hospital needs the (foot care) information. Because in there, they don’t have anyone who can give us any information.” (Participant 14, male, A1C 9%, a high-risk group)
“I know that there’s a lot of information, but no one publishes it…distributes it or publishes it via Facebook for people.” (Participant 24, male, A1C 7.4%, a high-risk group)
Subtheme 1.3 Communicate with plain language
According to the teaching/communication style, the participants showed difficulty understanding the foot care information that nurses provided because nurses often instructed patients using technical terms. Therefore, the participants prefer nurses to teach them easily without technical terms that might make it easy for them to understand the essential information as quoted below:
“… should be easily conveyed for understanding. Do not use professional language…use plain language…try to describe.” (Participant 24, male, A1C 7.4%, a high-risk group)
“Because I believe that (plain language) helps me to understand more about diet and having less illness” (Participant 20, female, A1C 7.6% a high-risk group)
Theme 2: Proactive Foot Screening with Foot Care Affirmation
Ambulatory care service and raising awareness for continual and consistent foot care are particular concerns for nurses. PWDs require community service, more public awareness, and affirmation for continuous foot caring, indicating that nurses should concern themselves with the holism of such patients, as shown in the quotes below:
“…should have PR. Should enhance awareness for patients. I fear having a foot ulcer. I am terrified. I think that we should be aware of this issue. It (foot ulcer) is terrifying because it (foot ulcer) is happening by accident. Even though I carefully monitor it, I am still forgetting to do it. It (foot ulcer) is terrifying. So, foot care is important.” (Participant 2, female, A1C 6.8%, a low-risk group)
“(Ambulatory care) goes outside (hospitals) to provide services.” (Participant 25, male, A1C 6.4%, a high-risk group)
“…need in-depth (foot caring) details because I know that only by accident, but I am not sure” (Participant 1, male, A1C 7.3%, a high-risk group)
Theme 3: Foot Care Services
Participants indicated that foot-care services were not adequately available. Some participants with financial problems need assistance from a hospital. For example, they reported that it would be beneficial if footwear accessories were reasonably priced and provided at a hospital because these necessary items would be easy to access and afford.
Subtheme 3.1 Easy access to foot care toolkits, footwear, and services
Accessibility to healthcare or foot care services is a need for PWDs in the low-risk and moderate groups because those patients suffer less severely from foot complications. Hence, they request health promotion services for foot ulcer prevention. Footcare toolkits, reasonable footwear prices, and suitable designs should be provided in hospitals because they are easy to access and beneficial for delaying foot complications. Besides, walking in for foot care services should be more concern, as enough staff at this center should be well-prepared for service as quoted below:
“I buy a curette…it (curette) is not good (quality)…I don’t know where I can buy a good one (curette)” (Participant 3, female, A1C 8%, a low-risk group)
“Footwear is pretty high in cost and unavailable for purchase outside a hospital…hospitals should sell it (footwear) for us” (Participant 11, male, A1C 8.7%, a high-risk group)
“Of course, we need easy-to-access footwear…and its (footwear) design should be good” (Participant 20, female, A1C 7.6%, a high-risk group)
“No need to be like me (having foot care appointments). Just walk in and get in the queue.” (Participant 2, female, A1C 6.8%, a low-risk group)
“It’s an unmatched appointment time. I visit a hospital, but (I) do not see any staff people” (Participant 8, male, A1C 8.6%, a moderate-risk group)
“In case of an abnormal symptom, for example, (I) have a foot ulcer that requires a foot exam. (I) need to access (a service)” (Participant 22, female, A1C 6.8%, a high-risk group)
Subtheme 3.2 Continuing Footwear Checking
Besides, the participants who needed footwear in the moderate group emphasized that they would like podiatrists to monitor their footwear closely; for example, the podiatrists should check both insole and outsole footwear (e.g., outsole breakdown) to prepare them for use as quoted below:
“…want them (doctors) to turn them face-up (outsole). Do not look only on the outside” (Participant 1, male, A1C 7.3%, a low-risk group)
“I want it (footwear) to cover my foot…it (foot) accidentally kicks sometimes…it (footwear) cracks. I have to use an old one (footwear) because they (doctors) do not fix it (footwear).” (Participant 3, female, A1C 8%, a low-risk group)
Themes 4: To Relieve Foot Burdens and Limb Loss
However, the patient needs of some participants in both the moderate and high-risk groups differed from the low-risk group. They would like to be treated by their doctors until their wounds healed, or they prefer that their doctors prevent any loss of their limbs, as shown in the quotes below:
“(I want a doctor) to cure (my foot ulcers until healed).” (Participant 7, female, A1C 7.1%, a moderate-risk group)
“(I want a doctor) to cure my diabetic foot ulcer” (Participant 8, male, A1C 8.6%, a moderate-risk group)
“(I want a doctor) to cure me until I’m healed. (I) don’t want to cut (my leg) off…..I want to heal. I’m discouraged.” (Participant 19, female, A1C 11.8% a high-risk group)
“(I want) my leg numbness to be gone.” (Participant 30, male, A1C 5.6% a high-risk group)
Discussion
This study has been aimed at exploring the needs of PWDs for both the prevention and treatment of diabetic foot complications. Four emerging themes highlighted that the needs of PWDs are different and similar in some issues, depending on the burden of foot complications and the severity of foot ulcer risk. Four significant themes regarding foot complication prevention and treatment are proposed. Each theme is discussed below.
Theme 1: Information Giving
Typically, nurses provide information to PWDs, enhancing low-education people’s knowledge, improving health behavior, or diabetes self-management (ElSayed et al., 2023c; Kaya & Karaca, 2018). On the other hand, deficient diabetes self-management results in poor quality nursing care (Nang et al., 2019; Ugwu et al., 2020) and poor health outcomes (Abbas, 2017; ElSayed et al., 2023b). In addition, nurses promote the quality of life for PWDs by preparing and supplying knowledge about foot care for preventing foot ulcers or delaying foot complications (Aalaa et al., 2017; Kanan et al., 2018). According to the literature review, foot care information alone may not be sufficient to promote self-confidence in PWDs, while good training for foot care until reaching patients’ confidence results in the management of abnormal symptoms and foot ulcer management (Kirk et al., 2023). Empowerment promotes self-confidence regarding foot care because nurses have more foot care information and are more experts than PWDs, in addition to trustable professionals. According to the 2023 ADA’s recommendations, Diabetes Self-Management Education Support (DSMES) is suitable for improved diabetes information, decision-making cultivation, and skill training, resulting in optimal diabetes outcomes (ElSayed et al., 2023c); however, DSMES in Thailand is not sufficiently established, especially decision-making and skill training. Nurses are supported to consider PWDs’ self-confidence for diabetes self-management (ElSayed et al., 2023c).
Multiple teaching strategies should be used during foot care training; for example, a foot care demonstration with re-demonstration should be provided for newly diagnosed PWDs (Nang et al., 2019), and recall techniques should be used for old-diagnosed patients. Most pieces of evidence recommended that all PWDs should be educated with skill training as soon as possible (Bus et al., 2020; ElSayed et al., 2023c) regarding self-assessment for early warning signs of foot complications (International Diabetes Federation, 2017) because up-skill/re-skill training, refreshment courses and coaching play a vital role in self-confidence, cultivating along the diabetes pathway in accordance with the ADA recommendations (ElSayed et al., 2023c).
Based on the emerging themes, some participants had information deficiency and limitations in information platforms. However, 80.7 percent of PWDs gain foot care knowledge, but refresher courses for reminding people of what they learned earlier provide sufficient knowledge (ElSayed et al., 2023a; Nang et al., 2019). Only single pieces of information are given to PWDs since they have been diagnosed with complications from diabetes, and this limitation results in their forgetting about their need for foot care. PWDs also request more detailed foot care/ulcer information, indicating that more explicit foot care information contributes to PWDs in terms of self-management with abnormality and delays further complications following the 2023 ADA’s recommendations, emphasizing an intensive diabetes self-management education (ElSayed et al., 2023a). Besides, some participants still remembered foot care information, and some of those participants learned from both their experience and a close relative's experience, indicating that they preferred to manage their symptoms without foot complications/ulcers by attempting to prevent foot complications as much as possible. Hence, foot care should consistently inform both PWDs who are with and without foot complications by process of integration into routine foot examinations (Begum et al., 2019; ElSayed et al., 2023a), combined with effective communication between PWDs and nurses (Patel et al., 2018; Pourkazemi et al., 2020).
The relationship between PWDs and healthcare providers is a cornerstone of enhanced self-management that has been emphasized for a long time (Polonsky et al., 2017), resulting in better health behaviors, diabetes self-management (ElSayed et al., 2023b), and effective glycemic control (White et al., 2015). The clear language used for diabetes self-management information and other support nurses deliver influences how well PWDs adapt to diabetes trajectory (Street Jr & Mazor, 2017). In addition, the evidence indicated that communication quality is also important because it can diminish diabetes distress, help patients better adapt to chronic illness, and improve adherence to diabetes care (Reeve et al., 2017).
Due to a shortage of nurses in Thailand, direct care involving providing time is limited because there is still an overwhelming workload, resulting in little effective communication between nurses and PWDs. A shortage of staff and an overwhelming workload are some of the barriers to healthcare service accessibility, leading to nurses being concerned only with the number of PWDs each day rather than the patients concerned (Kirk et al., 2023). Typically, PWDs request more time to cater to their needs or consult with nurses, but those nurses are unable to spend sufficient time for those purposes. It indicated that the nurses only provided a package of knowledge to the patients. However, it did so only after receiving less input from those patients, implying that a vicious cycle was still in progress.
Digital technology is a beneficial and seamless platform, especially in the post-COVID-19 era, as it can narrow the communication gap between nurses and PWDs. Digital technology supports those patients with easy-to-access foot care information from anywhere at any time and provides a platform for communication, counseling, and coaching per the 2023 ADA’s recommendations (ElSayed et al., 2023a). Multiple informational platforms through digital technology enhanced accessibility to essential foot care information for all diabetic foot ulcer risk groups and all age groups. Therefore, the already mentioned educational strategies contributed to PWDs in all risk groups of foot ulcers having various options for foot care management.
Theme 2: Proactive Foot Screening with Foot Care Affirmation
According to this theme, there are several reasons for increased proactive foot screening as follows: Firstly, foot care behavior among PWDs with a low risk of foot ulcer/complications is generally neglected by both nurses and PWDs, so both the Thailand Clinical Practice Guideline and the 2023 ADA’s Guidelines for foot complication prevention suggest foot examination at least annually for low to moderate risk groups (ElSayed et al., 2023c; Thai Ministry of Public Health, 2023) that is too long for foot complication monitoring.
Secondly, over 33.8 percent of hospitals in Thailand do not adhere to the National Guideline or any guideline (Kanan et al., 2021). Therefore, the Ministry of Public Health in Thailand should encourage hospitals at each level to adhere to clinical practice guidelines for better foot care management (Kanan et al., 2021).
Thirdly, less awareness of foot care in the low-risk group delays treatment in case of severe foot abnormality. A low-risk group will visit a hospital if foot complications are only presented (e.g., foot numbness, foot infection). Foot complications would be a concern when those complications affect the daily lives of those patients because PWDs and their relatives are unaware of foot care, which they typically ignore, resulting from only focusing on blood sugar control (Abbas, 2017). Only providing information is insufficient for a low-risk group in addition to being too late for foot complications prevention, which is why those participants mentioned that foot care awareness campaigns should be more promoted in society because over 85 percent of diabetic foot ulcers could be prevented (Corbett et al., 2019) by enhanced awareness and proper guidelines through increased public relations, including mass communication (Pourkazemi et al., 2020). Therefore, raising awareness of regular foot care for those patients is crucial because it is vital in eliminating the causes of foot problems (Monami et al., 2015).
Fourthly, ambulatory care or community proactive foot-care service should be promoted further because foot health promotion is better than foot ulcer treatment (Kanan et al., 2021). Services at this level contribute to those patients who do not access foot care services in hospitals (e.g., foot screening) (Nang et al., 2019). In addition, proactive foot care and screening should be more thoroughly addressed for nurses and related professions, while foot examinations should also be encouraged as daily routine care for all PWDs (Bus et al., 2020; ElSayed et al., 2023a). During a proactive foot screening or examination, nurses can provide and refresh foot care information in addition to foot care up-skill/re-skills for all risk groups of PWDs. For this reason, Thailand policymakers should focus on allocating a budget for foot examination—for example, budget allocation for foot examination training courses and refreshment courses for nurses—because early proactive foot examination and screening can delay severe foot complications or provide proactive treatment in communities in time for the prevention of worsening conditions.
According to foot care affirmation, nurses generally provide psychosocial support (e.g., empowerment, encouragement) to PWDs. If nurses are empowered, they can connect to those patients (Abbas, 2017; Nang et al., 2019), resulting in more confidence in the foot care of those patients. In addition, the psychosocial support during the provision of information by nurses also cultivates patient-nurse relationships with sincere communication (Kirk et al., 2023), resulting in improved health behavior or diabetes self-management (Kaya & Karaca, 2018). PWDs typically experience uncertainty because diabetes is a chronic condition that is unable to be treated, indicating that those patients live their lives with prolonged, unstable, and unpredictable health conditions. Those burdens and complicated diabetes self-management affect the psychosocial health status and well-being, including emotional distress, anxiety (ElSayed et al., 2023c), depression, guilt, and fear (Peimani et al., 2020; Pereira et al., 2019). Positive support can help PWDs have more self-confidence and high outcome expectations regarding foot examination, resulting in enhanced self-care and better foot care behaviors, as Bandura’s self-efficacy (Bandura, 1997).
Theme 3: Foot Care Services
Factors related to foot care development include a variety of footwear (Begum et al., 2019); however, some participants are struggling with a financial burden. Based on previous studies, economic status is primarily related to all dimensions of diabetes self-management (Birabwa et al., 2019; Ugwu et al., 2020). Financial problems are a significant barrier to healthcare-service accessibility because PWDs with foot complications or risks for foot ulcers have the responsibility for their foot care costs throughout their entire lives (e.g., footwear; treatment), including medical and non-medical costs, resulting in financial and healthcare-seeking burdens (Nang et al., 2019). In addition, those patients’ needs indicated a healthcare-service gap as a shortage of healthcare providers specializing in foot complications with work overloads leads to healthcare service inaccessibility (Birabwa et al., 2019; Pourkazemi et al., 2020). Participants reported that inadequate healthcare service access leads to a low level of foot care information and foot care behavior in accordance with a previous study (Kanan et al., 2018), even though the PWDs may have been informed about their need for foot care (Guell & Unwin, 2015). Therefore, nurses should emphasize working as a team with PWDs more.
Theme 4: Relieve Foot Burdens and Limb Loss
However, the participants from the moderate and high-risk groups mentioned that they would like the physician to treat their foot ulcers until their feet were fully healed, relieve foot numbness, and prevent amputation. This finding showed that some participants may misunderstand the subject of diabetes and its complications. PWDs should be aware that diabetes is a chronic and irreversible health condition. Suppose patients misunderstand this or are unable to accept it. In that case, the result can be an inability to live with a chronic illness, including experiencing fear and day-by-day challenges with obstacles along the way due to diabetes and its complications (Peimani et al., 2020). Essential information related to the causes of diabetes, self-management for foot ulcer prevention, and up-skills/re-skills are crucial factors in the area of foot care. Similarly, halting the progression of foot ulcers from poor self-management is a significant factor for nurses and patients in helping patients cope better and adhere to sound self-care principles (Ramkisson et al., 2017). Therefore, good adaptation to diabetes and accepting it as a manageable health condition facilitate living with well-being during a chronic illness, especially for the moderate to high-risk groups.
Psychological health status is one of the factors affecting the patients’ diabetes self-management ability, so those psychological factors should be monitored and screened as part of routine care at periodic intervals by trained nurses or collaborating with other well-trained healthcare providers (ElSayed et al., 2023c). The findings of the themes indicated that nurses should be more concerned with the psychosocial status of all PWDs as the 2023 ADA’s recommendations, especially for PWDs in both the moderate and high-risk groups. In a basic psychosocial status screening, nurses can apply informal questioning to screen for persistent mood changes within the previous two weeks or during the last appointment (ElSayed et al., 2023c). Therefore, nurses in the diabetes care team should report psychosocial issues (e.g., attitudes about diabetes, expectations for treatment, barriers to foot care) to a multidisciplinary team to resolve those psychosocial issues as a team collaboration.
Limitations
This study also struggled with some patient needs, which could not be manipulated only by nursing professionals. An effective working team, policy-makers’ considerations, and budget allocation are all required to improve foot care management in Thailand. The generalizability of these findings to other clinical settings should be a matter of concern because of the difference in the context of each setting. Also, the participants were purposively selected from only one university hospital. The selection of participants from only one university hospital imposed a limitation on this qualitative descriptive research.
Implications of the Study
The PWDs’ needs are incompatible with old-fashioned health education regarding foot care because the strategy to educate or provide support in Thailand does not exactly focus on patients’ needs but on information that nurses would like the patients to know. Therefore, nurses should reconsider how best to meet those needs in caring for and continuously understand PWDs to modify education strategies using the teaching-back method, reskill/upskill training, and coaching through diabetes self-management education and refreshment courses. Providing a variety of service platforms, both in-person and remote channels, is also necessary to ensure accessibility and affordability.
Conclusion
This descriptive qualitative study merged four themes reflecting the needs of PWDs. These patients’ needs indicated insufficiency and inaccessibility of foot care services in preventing and treating foot complications. In other words, the prevention and treatment of foot complications received by patients from nurses were still inadequate and mismatched with the patients’ needs. Therefore, this study’s findings could be used as preliminary information for clinical practice guidelines for diabetes mellitus improvement in terms of prevention and treatment of foot complications in Thailand based on nursing profession boundaries and the needs of the PWDs by modifying education strategies, providing refreshment courses, emphasizing holistic care and improving foot care information through various social media platforms.